Kerala’s Health department has released technical guidelines on the prevention, diagnosis and treatment of Amoebic meningoencephalitis.
- Kerala has reported five cases of Amoebic meningoencephalitis in adolescents in the past three months and with three deaths.
- The guidelines/standard operating procedure (SOP) is directed to be followed by all the hospitals when dealing with cases of acute meningitis.
About Amoebic Meningoencephalitis
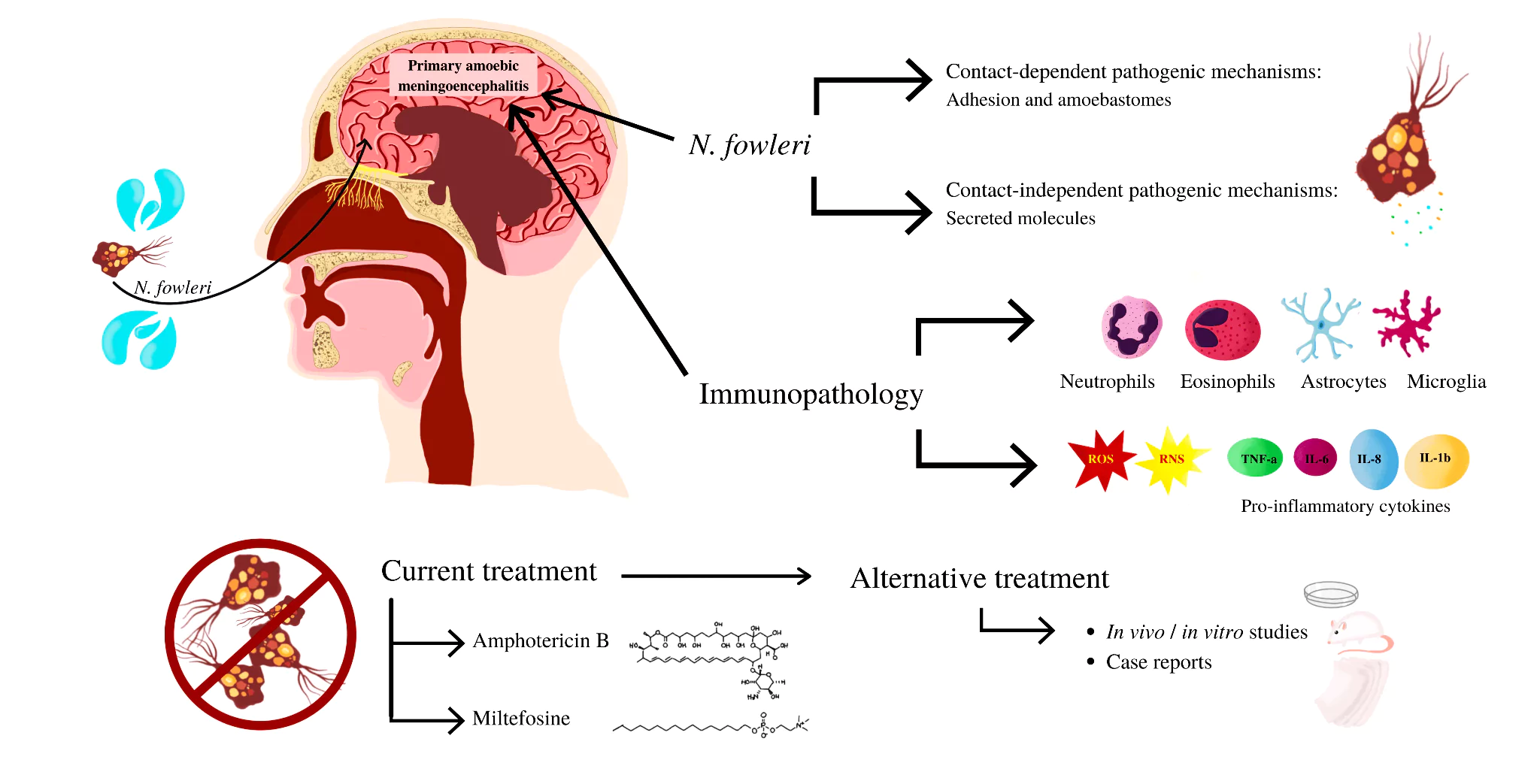
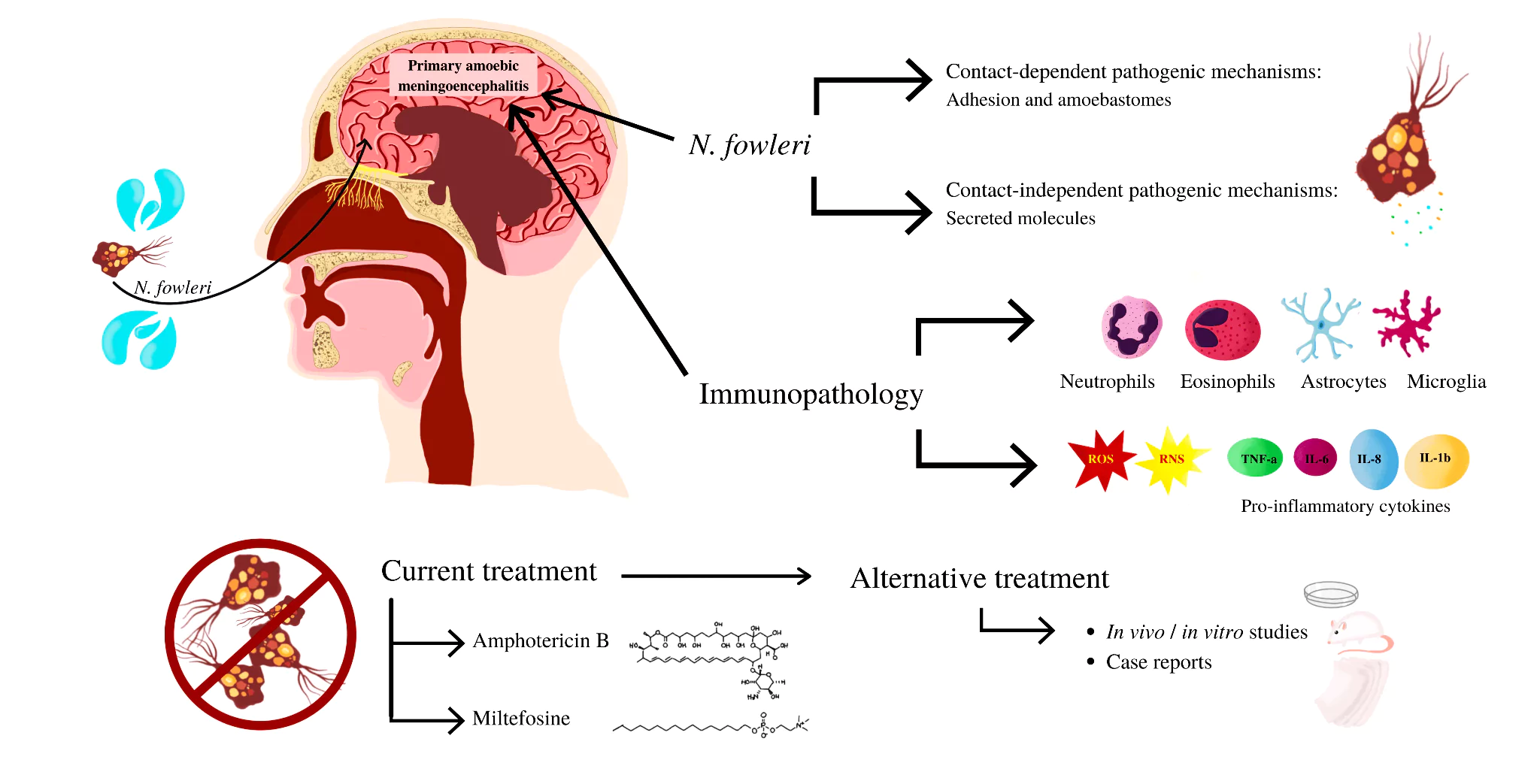
- It is a rare but lethal central nervous system (brain and spinal cord) infection caused by free-living amoebas found in freshwater, lakes, and rivers (never in seawater).
- This disease occurs more often during the warmer months of the year and in warmer climates.
- Exposure: The amoeba enters through the nasal channels and destroys brain tissue with patients typically having a history of swimming, diving, bathing, or playing in warm, generally stagnant, freshwater during the previous one to 9 days
- Types: There are two types of amebic encephalitis,
- Primary Meningoencephalitis (PAM):
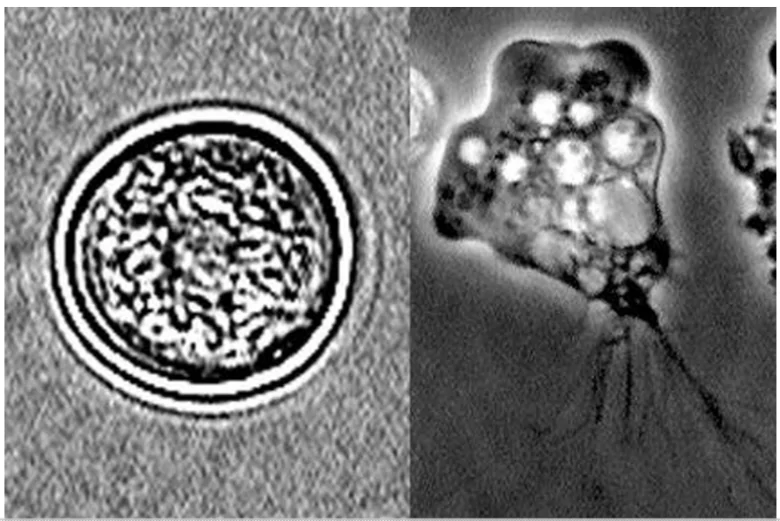
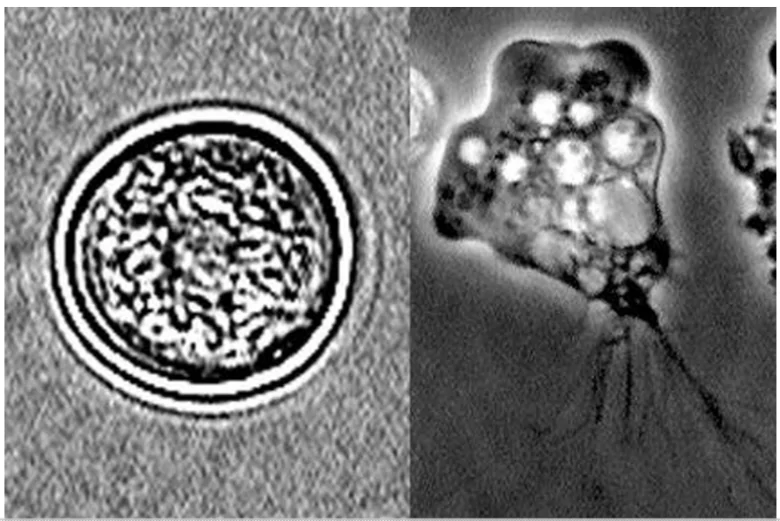
- Causative Agent: Naegleria fowleri, also known as a “brain eating ameba” and Vermamoeba Vermiformis.
- Symptoms: It began with a change in smell or taste which later progressed to headache, a stiff neck, sensitivity to light, nausea, and vomiting and seizures.
- The infection can progress rapidly, causing death within 10 days.
- Mortality Rate: PAM carries a high mortality rate of greater than 97% with only 11 survivors reported in the literature of the confirmed N fowleri PAM.
- Granulomatous Amebic Encephalitis (GAE):
- Causative Agent: Acanthamoeba species or Balamuthia mandrillaris.
- Symptoms: It can mimic a brain abscess, encephalitis, or meningitis.
- It usually occurs in people with a weakened immune system or generally poor health, and typically progresses more slowly than primary amebic meningoencephalitis.
- Early diagnosis: A spinal tap (lumbar puncture) is done to obtain a sample of cerebrospinal fluid (the fluid that surrounds the brain and spinal cord). This test can exclude some other possible causes of meningitis and brain infection, but doctors are not always able to find the amebas in the sample.
- Other Techniques to Detect Ameobas:
- Culture (growing microorganisms in a laboratory until there are enough to identify)
- Polymerase chain reaction (PCR) to check for the genetic material of the ameba
- A biopsy of brain tissue that is stained and examined under a microscope or analyzed using PCR
- Treatment: Timely initiation of an antimicrobial cocktail (Miltefosine) might be lifesaving with focus on a drug regimen consisting of an amebicidal drug (or a combination of drugs) with good in vitro activity that is capable of crossing the blood-brain barrier. There should be good supportive care also.
Enroll now for UPSC Online Course
Highlights of the SOPs On Amoebic Meningoencephalitis
- Tracing Patient History: Nasal exposure to fresh water in the 14 days before symptom onset should be asked of any patient who presents with symptoms of acute meningitis.
 Diagnosis: For meningitis patients with a history of recent nasal exposure to fresh water, the cerebro-spinal fluid (CSF) specimen should undergo rapid testing for N. fowleri/FLA .
Diagnosis: For meningitis patients with a history of recent nasal exposure to fresh water, the cerebro-spinal fluid (CSF) specimen should undergo rapid testing for N. fowleri/FLA .-
- Microbiologist should be immediately alerted about the clinical suspicion before sending CSF sample.
- Pre Treatment: PAM treatment should be considered for patients with clinical and CSF pictures suggestive of bacterial meningitis who are not responding to antibiotics or are rapidly deteriorating, even in the absence of exposure to fresh water.
- Treatment: All cases diagnosed as PAM through CSF microscopy should be immediately initiated on the recommended multi-drug regimen and supportive therapy aimed at lowering intracranial pressure.
- Team: All cases of PAM should be treated by a multidisciplinary team comprising physicians/paediatricians, intensivists, ID specialists, neurologists and microbiologists.
- Precautions to Follow:
- Avoid Water Bodies: One should avoid diving and jumping into stagnant water and keeping head above water when swimming in freshwater, hot springs, and other untreated thermal bodies of water.
- Limit Exposure: Use of nose plugs for unavoidable exposures, avoid digging, or stirring up the sediment when participating in water-related activities.
- Chlorination and proper maintenance of swimming pools/water theme parks, spas and daily emptying of wading pools
- Maintaining Nasal Hygiene: To ensure that water is not forcefully drawn into the nose during showering or washing face and using only filtered, or sterile water for nasal or sinus irrigation
Check Out UPSC CSE Books From PW Store
Naegleria Fowleri
- It is also known as a “brain eating ameba”
- Present In: It is found throughout the world in warm and shallow bodies of fresh water, such as lakes, rivers and hot springs. It also lives in soil but does not live in salt water.
- It also lives in hot springs or warm water discharged from industrial plants, poorly maintained swimming pools with minimal or no chlorination.
- It can even grow in water heaters at temperatures up to 115° F (46° C) and survive for short periods at higher temperatures.
- Free living organism: It is considered a free-living organism because it doesn’t need a host to live.
- Incubation Period: It takes about two to 15 days after you’ve been exposed to the amoeba for symptoms to develop.
|
![]() 23 Jul 2024
23 Jul 2024
 Diagnosis: For meningitis patients with a history of recent nasal exposure to fresh water, the cerebro-spinal fluid (CSF) specimen should undergo rapid testing for N. fowleri/FLA .
Diagnosis: For meningitis patients with a history of recent nasal exposure to fresh water, the cerebro-spinal fluid (CSF) specimen should undergo rapid testing for N. fowleri/FLA .