Recently, the Ministry of Health and Family Welfare released draft Guidelines for the Withdrawal of Life Support in Terminally Ill Patients to operationalise the Supreme Court’s 2018 and 2023 orders on the right to die with dignity for all Indians.
About Terminally ill
- Terminally ill is a condition where a person has an incurable illness or malady that will ultimately result in their death.
- People with terminal illness often will undertake a series of financial and administrative tasks in order to settle their financial obligations and allocate assets to their beneficiaries upon death.
|
Enroll now for UPSC Online Course
About Draft Guidelines for the Withdrawal of Life Support
- Issued by: Ministry of Health and Family Welfare.
- Objective: Operationalise the Supreme Court’s 2018 and 2023 orders on the right to die with dignity under Article 21 (Right to life and personal liberty).
- Legal Recognition: Withholding/withdrawing life-sustaining treatment is legal in India under a structured framework, though there’s no specific legislation on this.
Key Mechanisms
- Medical Boards:
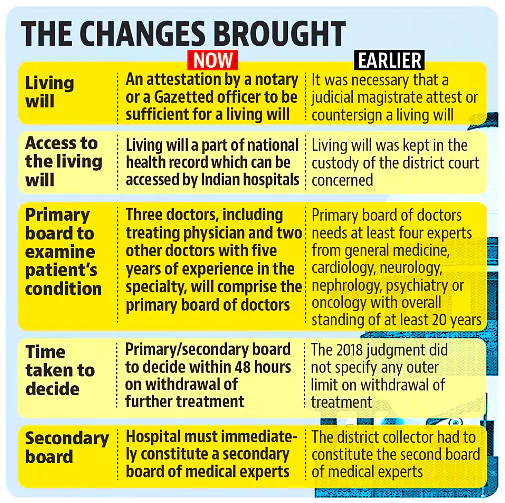
- Primary Medical Board: Composed of the treating doctor and two experts, it determines if further treatment is beneficial.
- Secondary Medical Board: Confirms or rejects the Primary Board’s decision, includes members nominated by the district Chief Medical Officer.
- Living Will/Advance Medical Directive:
- A written document for individuals aged 18+, specifying end-of-life treatment preferences if they lose decision-making capacity.
- Requires at least two surrogate decision-makers and must be signed, witnessed, and attested.
- Do-Not-Attempt-Resuscitation (DNAR) Orders:
- Issued by the treating physician with family/patient consent.
- Limits resuscitation efforts but continues other medical treatments for comfort.
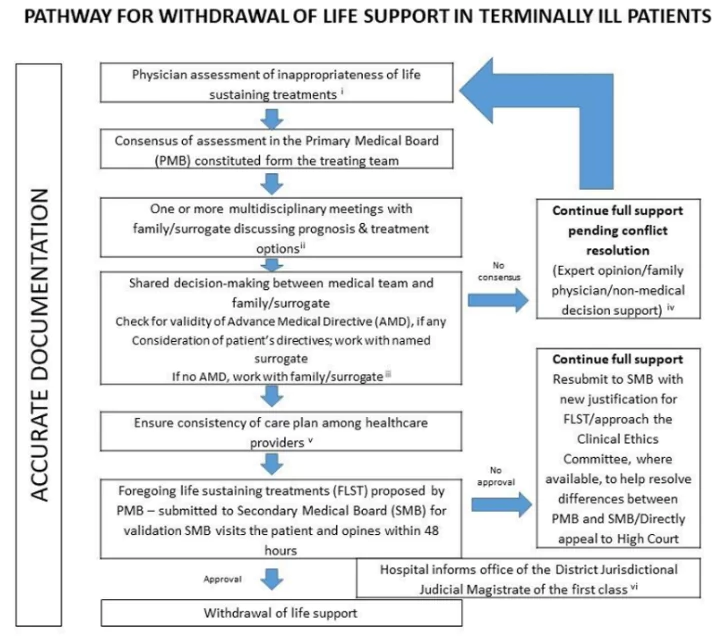
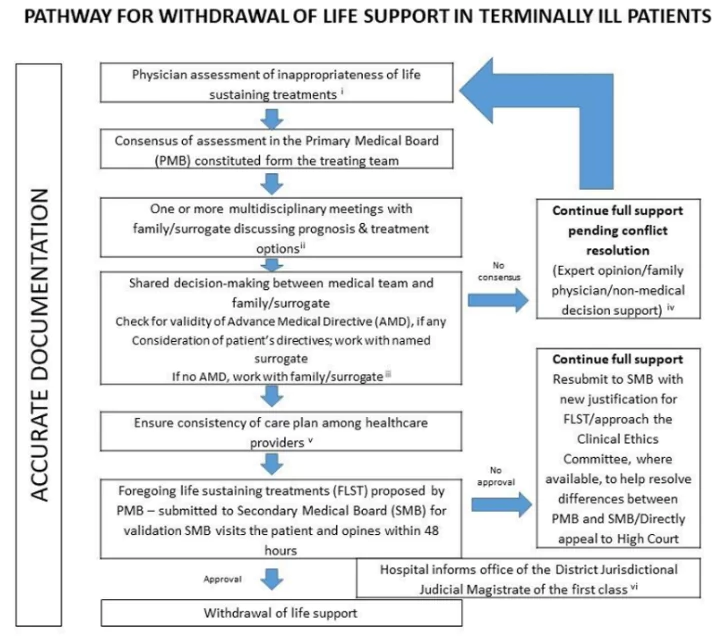
- Process of Withholding/Withdrawing Treatment
- Assessment:
- The Primary Medical Board assesses the patient’s condition.
- The Secondary Medical Board reviews the recommendation for another level of checks.
- Consent and Notification:
- Requires the consent of the patient’s nominated surrogate decision-makers.
- Decisions must be notified to the local judicial magistrate.
- Ethical and Practical Considerations
- Shared Decision-Making: Ensures joint decisions between medical teams and families, upholding patient autonomy and legal clarity.
- This approach provides legal protection for doctors, honours the patient’s autonomy, incorporates family preferences, and upholds ethical standards, ensuring that responsibility does not rest solely on the physician.
- Palliative Care: Focuses on managing pain and providing comfort when life-support is withdrawn, not considered as giving up on the patient.
- Passive Euthanasia Misinterpretation: “Passive euthanasia” refers to withholding/withdrawing life-sustaining treatment, distinct from active euthanasia, which is intentional killing for mercy.
About Euthanasia
- Refers: The practice under which an individual intentionally ends his/her life to get relief from an incurable condition, or intolerable suffering.
- Etymology: The word ‘euthanasia’ is a product of two Greek words ‘eu’ meaning ‘good’ and ‘thanatos’ meaning ‘death’.
- Types of Euthanasia: There are four types of euthanasia.
- Active euthanasia: It involves an active intervention to end a person’s life with substances or external force, such as administering a lethal injection.
- Passive euthanasia: It refers to withdrawing life support or treatment that is essential to keep a terminally ill person alive.
- Voluntary euthanasia: It takes place with the consent of the patient.
- Involuntary euthanasia: It is administered without the patient’s consent.
Suicide v/s Euthanasia
- Suicide is the intentional act of ending one’s own life, often due to reasons like despair or depression.
- In contrast, euthanasia, or “mercy killing,” involves another person ending the life of someone who is terminally ill, based on the belief that their quality of life has deteriorated to the point where death would be a compassionate choice for medical reasons.
|
SC judgement related to Right to Life and Right to Die
- Maruti Sripati Dubal vs. State of Maharashtra (1987)
- Context: Petitioner attempted suicide, was charged under Section 309 of the Indian Penal Code (IPC), 1860.
Check Out UPSC CSE Books From PW Store
Customary Religious Practices:
- Prayopavesa (literally resolving to die through fasting) is a practice in Hinduism that denotes the suicide by fasting of a person who has no desire or ambition left, and no responsibilities remaining in life.
- A similar practice exists in Jainism, termed Santhara.
- In Tamil culture, it is called Vatakkiruttal and Sokushinbutsu in Buddhism.
|
-
- Judgement: Declared Section 309 unconstitutional as it was harsh and unreasonable. Emphasized the need for mental health support rather than penal action against individuals attempting suicide.
- Rathinam vs. Union of India (1994)
- Judgement: Supreme Court upheld Maruti Sripati Dubal’s decision, declaring the Right to Life under Article 21 also includes the Right to Die.
- Gian Kaur vs. State of Punjab (1996)
- Reversal: Five-judge Constitutional Bench overruled the Rathinam case.
- Ruling: Right to Life does not include the Right to Die. Section 309 of IPC was deemed constitutional, affirming that suicide is not a protected liberty under Article 21.
241st Law Commission Report on Euthanasia
- The 241st Law Commission Report, titled “Passive Euthanasia – A Relook,” presents several key observations on euthanasia.
- It asserts that both euthanasia and assisted suicide should remain illegal in India, while recommending that withdrawal of life support be allowed for individuals in a persistent vegetative state, irreversible coma, or those lacking decision-making capacity.
- The report emphasizes that medical professionals should act in the patient’s best interests and recognizes the right of conscious, competent terminally ill patients to refuse life-prolonging treatments, acknowledging that modern medical interventions may lead to significant pain and suffering.
|
SC on Euthanasia In India
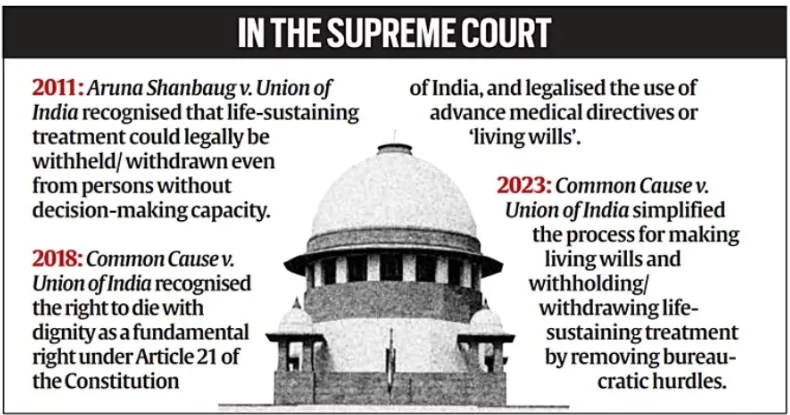
- Aruna Ramchandra Shanbaug v. Union of India (2011): In this case, the Supreme Court had held that passive euthanasia can be allowed under exceptional circumstances.
- Common Cause vs. Union of India (2018): The Supreme Court allowed passive euthanasia while recognising the living wills of terminally-ill patients who could go into a permanent vegetative state, and issued guidelines regulating this procedure.
- Living Will: A living will is a legal document that specifies the type of medical care that an individual does or does not want in the event they are unable to communicate their wishes.
- It is also known as an advance directive.
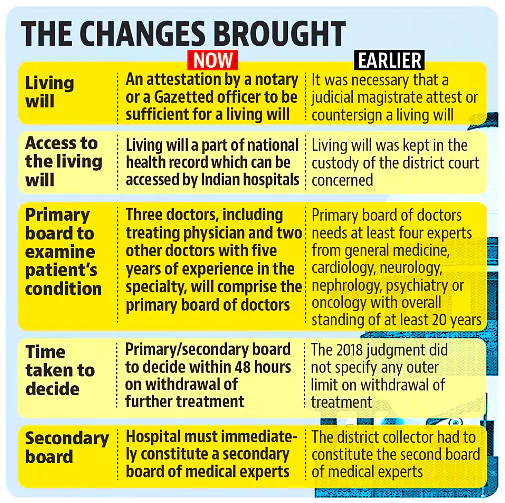 In 2023 the Supreme Court modified the guidelines to make the right to die with dignity more accessible.
In 2023 the Supreme Court modified the guidelines to make the right to die with dignity more accessible.
Check Out UPSC NCERT Textbooks From PW Store
Global Trends
- Netherlands, Luxembourg, Belgium: These Countries allow both euthanasia and assisted suicide for anyone who faces “unbearable suffering” that has no chance of improvement.
- Switzerland: Switzerland has banned euthanasia but allows assisted dying in the presence of a doctor or physician.
- Canada: Canada had announced that euthanasia and assisted dying would be allowed for mentally ill patients by March 2023; however, the decision has been widely criticised, and the move may be delayed.
- United States: USA has different laws in different states. Euthanasia is allowed in some states like Washington, Oregon, and Montana.
- United Kingdom: The United Kingdom considers it illegal and equivalent to manslaughter.
- In 2021, Australia, New Zealand, Spain, and Portugal passed legislation to legalise or adopt euthanasia.
- Australia: New South Wales, Queensland, South Australia, Tasmania, Victoria, and Western Australia allowed voluntary assisted dying (VAD)
- New Zealand: Euthanasia is legal, but a national referendum on the issue will take place in September 2020
- Portugal: Law is not yet in force, but is awaiting regulation
Ethical Dimensions of Euthanasia
- Respect for Autonomy and Informed Consent: Euthanasia prioritises individual autonomy, allowing mentally competent individuals to make decisions about ending their suffering.
- Full informed consent is necessary to ensure the individual fully understands their condition and options.
- Balancing Quality of Life with Sanctity of Life: The debate centres on quality of life, where ending suffering and preserving dignity are prioritised, versus sanctity of life, which views life as inherently valuable and not to be ended prematurely.
- Implications for Law and Society: Euthanasia regulations vary widely by jurisdiction, reflecting different cultural and ethical views.
- Socially, euthanasia raises questions about the role of medical professionals, societal responsibilities, and the accessibility of palliative care.
Significance of the Guidelines
- Strengthening the Right to Die with Dignity: These guidelines put into action the Supreme Court’s 2018 and 2023 decisions in the Common Cause case,
- It firmly establishes the legal right for terminally ill patients to pass with dignity under Article 21.
- Establishing a Framework for Decision-Making: Guidelines require hospitals to form Primary and Secondary Medical Boards.
- It provides oversight to ensure that decisions to withdraw life support are carefully reviewed and responsibly enacted.
- Defining Clear Procedures for Life Support Withdrawal: The guidelines detail a clear process: the Primary Board assesses, the Secondary Board independently reviews, consent from designated surrogates is obtained, and judicial notification is completed.
- This framework ensures transparency and accountability.
- Emphasising Ethical, Collaborative Decision-Making: Encourages collaboration between the medical team and the patient’s family.
- It aligns treatment with the patient’s wishes, protecting medical professionals legally, and easing the decision-making burden on families.
Check Out UPSC Modules From PW Store
Challenges with the Guidelines
- Complexity in Medical Board Formation: Setting up Primary and Secondary Medical Boards in every hospital can be resource-intensive, particularly for smaller or rural hospitals with limited facilities and personnel.
- Absence of Specific Legislation: Without a dedicated law on the Right to Die, implementation might be inconsistent, leading to legal ambiguities. This could discourage hospitals from applying the guidelines comprehensively.
- Terminological Confusion: Continued use of terms like “passive euthanasia” may create social discomfort and misunderstandings, potentially hindering societal acceptance of the right to die with dignity.
- Complicated Living Will Process: The process of creating a living will is complex, involving documentation, witnesses, executors, and notary verification, which could make it inaccessible to many people.
- Potential Delays in Decision-Making: The multi-step process—medical board assessments, family consent, and judicial notification—might slow decision-making, delaying timely withdrawal and impacting the right to die with dignity.
- Emotional and Ethical Burden on Families and Doctors: Shared decision-making, although essential for patient rights, places significant emotional strain on families and an ethical burden on physicians.
Way Forward
- Legislative Action to Provide Clarity: Lawmakers should consider drafting specific legislation on life-support withdrawal in terminal cases, providing a robust legal framework to support the right to die with dignity.
- Training and Awareness for Medical Professionals: Medical staff should receive training on the ethical, legal, and procedural aspects of life-support withdrawal to enhance their understanding and approach to end-of-life care.
- Simplifying the Living Will Process: Streamlining the procedure for creating and verifying a living will could make it more accessible to people across different backgrounds.
- Public Education and Awareness Initiatives: Educating the public on end-of-life choices will help families make well-informed decisions aligned with their loved ones’ wishes, fostering understanding and reducing unnecessary suffering.
- Strengthening Palliative Care Services: Expanding access to quality palliative care across hospitals and healthcare centers can offer terminally ill patients comfort and relief from suffering, ensuring that their remaining life is as pain-free as possible.
- Building Support Systems for Families and Caregivers: Providing psychological counselling and support for families and caregivers
- It can help them navigate the emotional and ethical challenges associated with end-of-life decisions, reducing stress and ensuring compassionate care for patients.
Enroll now for UPSC Online Classes
Conclusion
- The guidelines for life-support withdrawal mark a crucial step towards recognizing the right to die with dignity, balancing legal clarity, patient autonomy, and ethical medical practice.
- By addressing legislative gaps, enhancing public awareness, and strengthening support systems, India can ensure a compassionate, well-structured approach to end-of-life care.
![]() 28 Oct 2024
28 Oct 2024

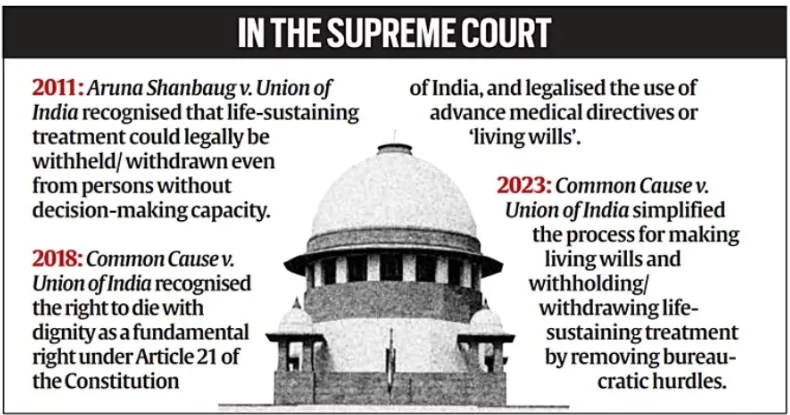
 In 2023 the Supreme Court modified the guidelines to make the right to die with dignity more accessible.
In 2023 the Supreme Court modified the guidelines to make the right to die with dignity more accessible.