A study published in The Lancet Infectious Diseases revealed that only 7.8% of patients with drug-resistant infections in India received appropriate antibiotics, compared to an average of 6.9% across eight low- and middle-income countries (LMICs).
The study examined 1.5 million cases of carbapenem-resistant Gram-negative (CRGN) infections in countries including India, Bangladesh, Brazil, Egypt, Kenya, Mexico, Pakistan, and South Africa.
About Carbapenem-resistant Gram-negative (CRGN)
- Carbapenem-resistant Gram-negative (CRGN) infections are caused by bacteria that are resistant to carbapenems, a class of last-resort antibiotics.
- These infections are extremely difficult to treat, leading to high mortality rates, prolonged hospital stays, and increased healthcare costs.
- They can only be treated using newer generation antibiotics such as ceftazidime-avibactam, colistin, tigecycline, and fosfomycin.
|
Key Highlights of Study
- Conducted by: the Global Antibiotic Research and Development Partnership (GARDP)
- Objective: To identify barriers from health facility presentation to diagnostic testing and access to effective treatment.
- It used data from The Lancet’s Global Burden of AMR (GRAM) study and IQVIA , 2019.
- Data Base: The research assessed data from eight populous low- and middle-income countries (LMICs): India, Bangladesh, Brazil, Egypt, Kenya, Mexico, Pakistan, and South Africa.
- High Burden in India: In 2019, India recorded nearly 10 lakh carbapenem-resistant Gram-negative (CRGN) infections, but less than 1 lakh patients received appropriate treatment.It also found that only 7.8% of patients in India with CRGN infections received appropriate antibiotics
- The study estimates around 3.5 lakh deaths in India due to inadequate treatment of these infections.
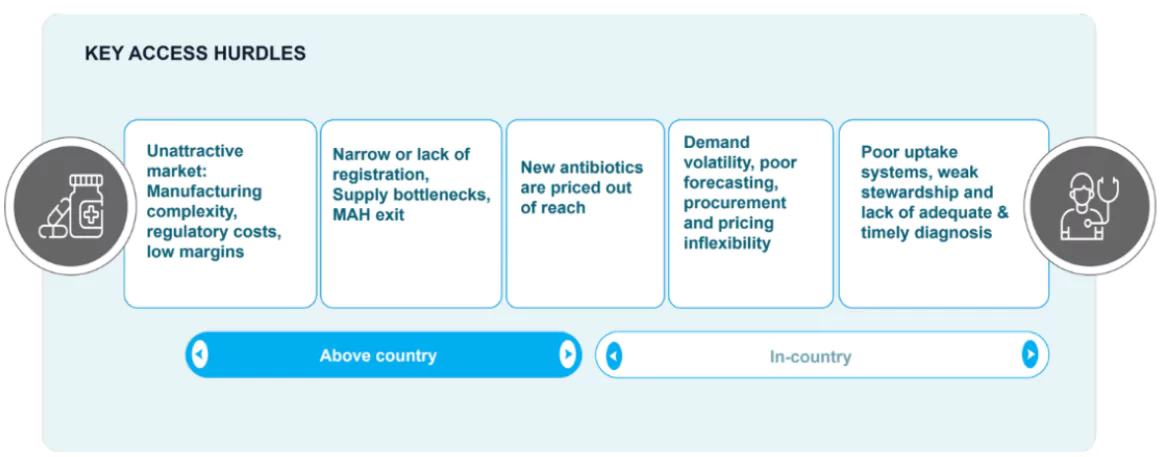
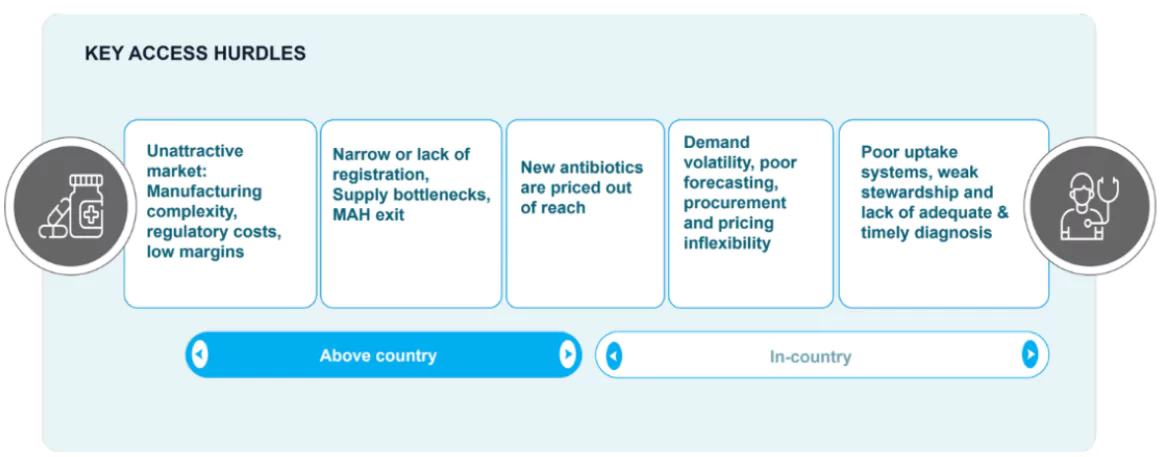
Challenges Regarding Access to Antibiotics
- Paradoxical challenge: Country like India faces paradoxical challenges of irrational overuse of high-end antibiotics on one hand, and limited access to them for those in genuine need on the other.
| PWOnlyIAS Extra Edge
Working Group 4 (WG4): The NMP is composed of four time-limited working groups (WGs) following the themes of transparency, solidarity, sustainability and novel antimicrobials. |
- Supply Chain Issues: Access is hindered due to intermittent shortages when demand outpaces supply and Marketing Authorisation Holder (MAH) withdrawal of antimicrobials from markets for economic reasons, especially in LMICs.
- Lack of Infrastructure: Many patients are not diagnosed properly due to underdeveloped lab infrastructure and lack of awareness, leading to delays or absence of appropriate treatment initiation.
- PolicyGaps: Weak antibiotic stewardship programmes and absence of effective regulatory guardrails contribute to both misuse and access failures, aggravating antimicrobial resistance (AMR).
Global Initiatives to Improve Access to Antibiotics
- WHO Novel Medicines Platform (NMP): Launched in April 2024, the NMP aims to ensure sustainable innovation of novel antibiotics and enhance access to existing ones.
- Working Group 4 (WG4): NMP’s WG4 plans to develop multistakeholder proposals to improve antibiotic access, focusing on regulatory, financial, and supply chain solutions.
- SECURE Global Initiative: SECURE, developed by WHO and GARDP with UNICEF and CHAI, aims to expand antibiotic access for LMICs, ensuring rational and equitable use of antimicrobials.
Additional Reading: AMR
![]() 1 May 2025
1 May 2025