Out-of-Pocket Expenditure (OOPE) has long strained Indian households, driving many into poverty.
About Out-of-Pocket Expenditure (OOPE)
- Definition: Refers to direct payments by households for healthcare services such as doctor consultations, medicines, diagnostics, and hospital stays, without reimbursement.
- Nature of Spending: Often includes non-subsidized drugs, diagnostic tests, and hospitalization charges, making it a heavy financial burden.
- Policy Relevance: High OOPE is considered an indicator of weak public health financing and low insurance penetration.
Key Findings by National Health Accounts estimates released by the Ministry of Health and Family Welfare for 2021-22
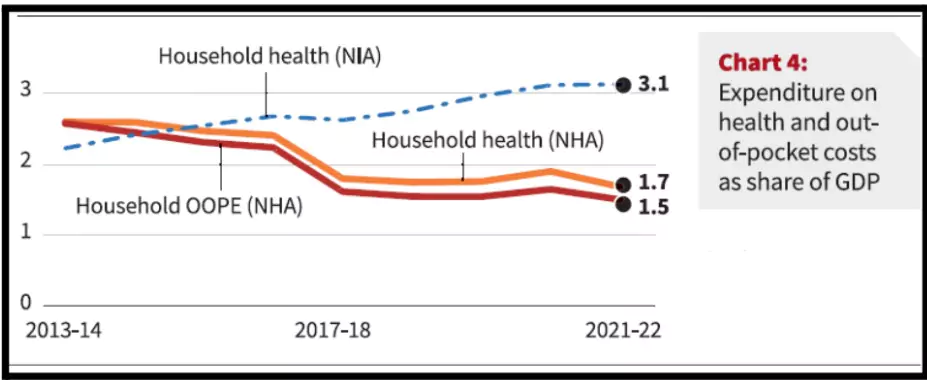
- OOPE Decline: OOPE reduced to 39.4% of total health expenditure (THE) in 2021-22 from 48.8% in 2017-18.
- Government’s Share Increase: Government’s share in THE rose from 40.8% to 48%.
- Goal: OOPE to be reduced to 35% of THE by 2025-26.
Total Health Expenditure (THE):
- Total Health Expenditure (THE) refers to the sum of all public and private spending on health services within a country over a specific period. It includes government spending, insurance payments, and out-of-pocket expenditure by households.
|
Status of OOPE in India
- As per Economic Survey 2024-25, India’s OOPE is 39.4%, making healthcare unaffordable for many.
- Countries like the UK & Australia have approx 13% OOPE, as they rely on public healthcare systems.
Key Drivers of Decline in OOPE
- Increased Government Health Expenditure (GHE): Share of GHE rose from 1.13% of GDP (2014-15) to 1.84% (2021-22), making public care more affordable.
- Expansion of Social Security Expenditure (SSE): Share increased from 5.7% to 8.7% of Total Health Expenditure (THE), offering protection from catastrophic spending.
- Targeted Programs for Non-Communicable Diseases (NCDs): Subsidized initiatives for diabetes, hypertension, and cancer treatment reduced long-term household health costs.
 COVID-19 Response: Investments in testing, oxygen plants, ICU beds, and vaccines built lasting infrastructure, indirectly lowering OOPE.
COVID-19 Response: Investments in testing, oxygen plants, ICU beds, and vaccines built lasting infrastructure, indirectly lowering OOPE.
- Public Health Infrastructure & Workforce: Establishment of Ayushman Arogya Mandirs, better-equipped district hospitals, and trained health staff expanded affordable access.
- Ayushman Arogya Mandirs (AAMs): 1.76 lakh centres delivering preventive, promotive, curative, palliative, and rehabilitative services, making care universal and free closer to communities.
- Policy Interventions:
 National Health Mission (NHM): Strengthening state healthcare infrastructure, human resources, and services for underserved groups.
National Health Mission (NHM): Strengthening state healthcare infrastructure, human resources, and services for underserved groups.- National Free Drugs and Free Diagnostic Services: Ensuring availability of essential medicines and tests, cutting OOPE for patients at public facilities.
- Pradhan Mantri Ayushman Bharat Health Infrastructure Mission (PM-ABHIM): ₹64,180 crore outlay to build capacity in primary, secondary, and tertiary healthcare.
 Government-Funded Insurance Schemes: Initiatives like Ayushman Bharat–PMJAY and state health schemes cover hospitalization costs for vulnerable groups.
Government-Funded Insurance Schemes: Initiatives like Ayushman Bharat–PMJAY and state health schemes cover hospitalization costs for vulnerable groups.
- Ayushman Bharat–Pradhan Mantri Jan Arogya Yojana (AB-PMJAY): Provides ₹5 lakh cover per family per year for secondary and tertiary care to 55 crore beneficiaries (12.37 crore families) representing the bottom 40% of India’s population. Recently expanded to cover 6 crore senior citizens (70+ years) irrespective of socio-economic status.
- Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP) and Affordable Medicines and Reliable Implants for Treatment (AMRIT) pharmacies: Ensuring access to quality generic medicines at affordable prices.
Implications of Reduced OOPE
- Improved Healthcare Accessibility: Households, especially in rural and low-income areas, can now seek treatment without major financial barriers.
- Strengthened Public Health System: Higher funding has improved resource distribution and service reliability in government facilities.
- Better Health Outcomes: Preventive care and early diagnosis lower morbidity and mortality, easing system-wide burden.
- Financial Stability for Families: Reduced spending on health frees resources for nutrition, education, and household resilience.
- Boost for Health Workforce: Greater government expenditure enables recruitment and training of doctors, nurses, and paramedics, improving service delivery.
- Pathway to Universal Health Coverage (UHC): Declining OOPE strengthens India’s progress towards SDG 3 (Good Health & Well-being) and the vision of healthcare as a right.
About National Health Accounts (NHA)
- NHA tracks the flow of health resources in a country, analyzing spending, funding sources, and resource distribution across sectors.
- Key Elements of NHA:
- Health Expenditure Tracking: Breaks down spending from government, private insurance, OOPE, and foreign aid.
- Sources of Funding: Tracks funding from government, social health insurance, private sector, and household spending.
- Service Areas: Categorizes spending on hospital care, outpatient services, pharmaceuticals, etc.
- System Insights: Helps assess efficiency and equity in healthcare financing.
- Performance Monitoring: Tracks financial sustainability and informs decisions to improve health outcomes.
- NHA Frameworks and Standards:
- The System of Health Accounts (SHA) by Organisation for Economic Co-operation and Development (OECD) and the World Health Organization (WHO) is the international standard for NHA, regularly updated to reflect new trends in health financing.
NHA in India
- India’s NHA tracks public and private healthcare spending, informing the country’s progress toward Universal Health Coverage (UHC).
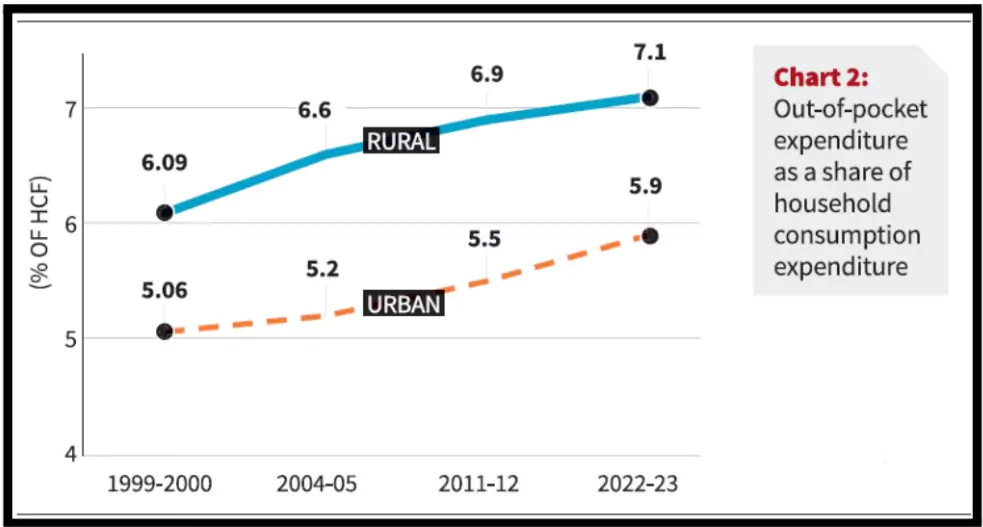
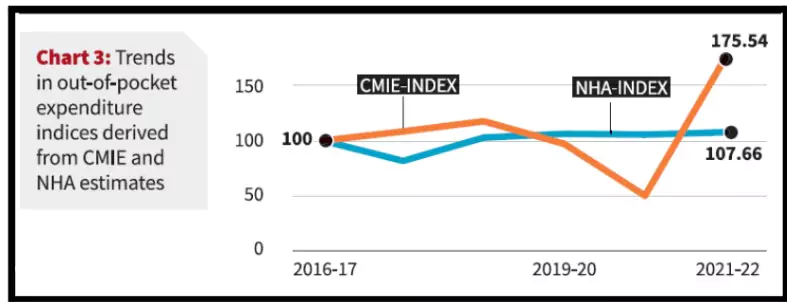
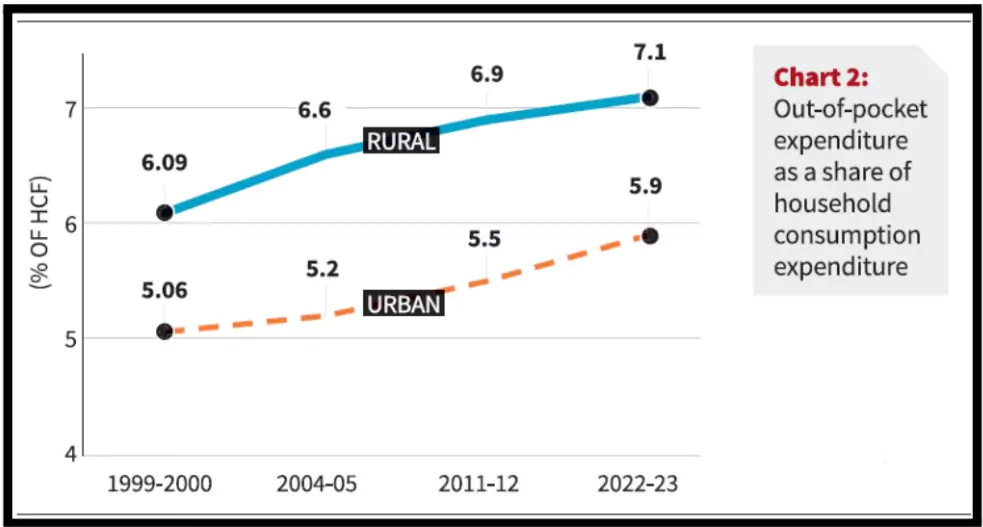
- Trends: OOPE declines in NHA, but CPHS shows slower reductions, especially post-COVID.
- Significance: Informs health financing targets, like increasing public health spending to 2.5% of GDP.
|
Challenges of Out-of-Pocket Expenditure (OOPE)
- Financial Burden on Families: High OOPE forces households to dip into savings, borrow, or sell assets, diverting resources from food, education, and livelihoods, often leading to catastrophic health expenditure.
- Example: World Health Organization (WHO) 2022 reports families spend 10–25% of income on healthcare, pushing many into poverty traps.
- Equity in Access: Schemes like AB-PMJAY mainly cover hospitalisation, leaving outpatient care and medicines—the majority of OOPE—uncovered.
- Example: Lancet Report 2023 found medicines alone account for over 60% of OOPE, disproportionately burdening rural poor.
- Rising Cost of Healthcare: Prices of diagnostics, medicines, and treatments continue to rise despite government initiatives.
- Example: NPPA 2024 reported a 12% increase in essential drug prices, escalating household financial strain.
- Data Reliability: Over-reliance on NSS 2017-18 and extrapolated NHA estimates undermines accuracy.
- Example: NITI Aayog 2021 highlighted inconsistencies between NHA and National Income Accounts estimates of household health spending.
- COVID-19 Expenditure Shock: Pandemic-related costs for oxygen, hospital beds, and medicines were largely borne out-of-pocket and not captured in NHA.
- Example: Azim Premji University 2022 estimated 200 million Indians pushed into poverty due to healthcare spending.
- Low Public Health Spending: At 1.84% of GDP, India’s public health expenditure remains below the WHO benchmark of 5%, limiting protection from OOPE.
- Example: Economic Survey 2023-24 emphasized raising GHE to 2.5% of GDP by 2025 as per National Health Policy 2017.
Way Forward
- Strengthen Health Data Systems: Integrate multiple surveys (NSS, NFHS, CES, LASI, CPHS) to create a composite, real-time NHA.
- Expand Coverage Beyond Hospitalisation: Extend AB-PMJAY and state schemes to include outpatient care, diagnostics, and medicines, the main drivers of OOPE.
- Regulate and Reduce Medicine Prices: Scale up Pradhan Mantri Bhartiya Janaushadhi Pariyojana and strengthen drug price regulation through National Pharmaceutical Pricing Authority.
- Pandemic-Responsive Financing: Develop emergency health financing mechanisms and expand insurance coverage for epidemics.
- Increase Public Health Spending: Raise Government Health Expenditure (GHE) to at least 2.5% of GDP by 2025 as per National Health Policy, and move closer to WHO-recommended 5%.
Conclusion
The reduction in Out-of-Pocket Expenditure (OOPE) aligns with India’s commitment to SDG 3 (Good Health and Well-being), ensuring universal health coverage and equitable access to quality healthcare services. Continued government investment, inclusive insurance schemes, and a focus on health equity are essential to achieving long-term healthcare sustainability.
Read More About: Union Budget 2025 on Public Healthcare
Read More About: Health Insurance In India
![]() 18 Sep 2025
18 Sep 2025

 COVID-19 Response: Investments in testing, oxygen plants, ICU beds, and vaccines built lasting infrastructure, indirectly lowering OOPE.
COVID-19 Response: Investments in testing, oxygen plants, ICU beds, and vaccines built lasting infrastructure, indirectly lowering OOPE.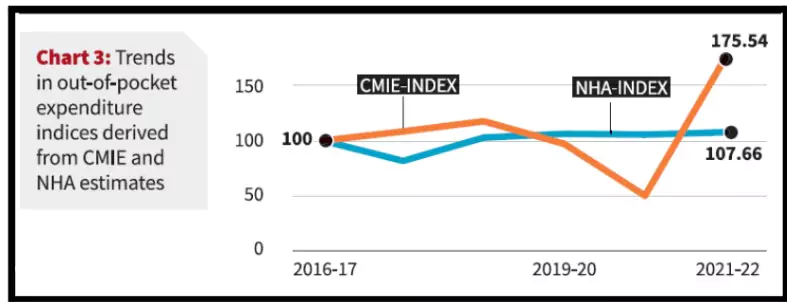 National Health Mission (NHM): Strengthening state healthcare infrastructure, human resources, and services for underserved groups.
National Health Mission (NHM): Strengthening state healthcare infrastructure, human resources, and services for underserved groups.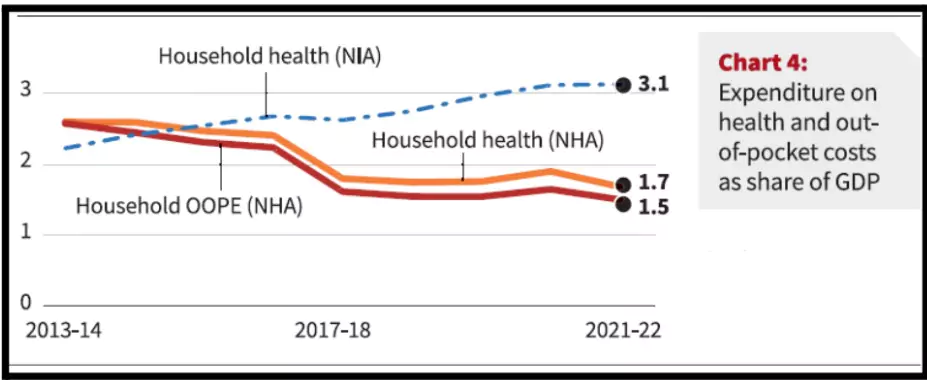 Government-Funded Insurance Schemes: Initiatives like Ayushman Bharat–PMJAY and state health schemes cover hospitalization costs for vulnerable groups.
Government-Funded Insurance Schemes: Initiatives like Ayushman Bharat–PMJAY and state health schemes cover hospitalization costs for vulnerable groups.