Context:
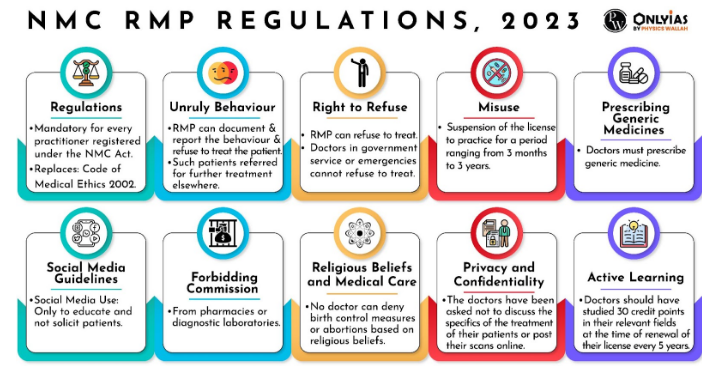
According to the National Medical Commission’s Registered Medical Practitioner (Professional Conduct) Regulations or NMC RMP Regulations 2023, doctors can now refuse treatment to the unruly and violent patients.
About The National Medical Commission Act, 2019:
- It was introduced to address various issues and challenges in the medical field, including improving the quality of medical education, enhancing access to healthcare services, and ensuring ethical and transparent practices.
- Key Provisions include:
- Ethical and Professional Conduct: The Act emphasizes maintaining ethical and professional conduct among medical practitioners and includes provisions to address any deviations from these standards.
- Community Health Providers: The Act introduces the concept of Community Health Providers who are allowed to practice limited medicine in underserved rural areas to address the shortage of doctors.
- Formation of the National Medical Commission (NMC): NMC is an regulatory body which regulates medical education and medical professionals.
- Establishment of Medical Advisory Council.
- Reforms in Medical Education.
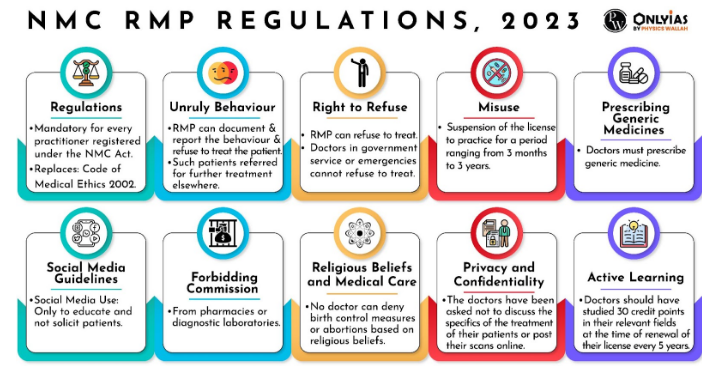
Refusing treatment is a complex issue that involves various stakeholders viz. doctors and healthcare professionals, patients and their families, healthcare institutions, medical associations and regulatory bodies, legal authorities, ethics committees, public opinion and media, religious and cultural communities, etc.
Arguments in Favour of the Regulation:
- Unruly Behaviour
- Justice: If an unruly patient’s behaviour poses a threat to their own safety, the safety of healthcare staff, or the safety of other patients, refusing treatment might be justified as a means to mitigate these risks.
- For example, a 21-year-old patient attacked a doctor with a knife during consultation at Delhi’s Sir Ganga Ram Hospital.
- Dignity and Integrity: Unruly behaviour can sometimes cross ethical boundaries, leading to disrespectful or abusive treatment of healthcare staff. Doctors have a right to work in an environment that respects their dignity and professional integrity.
- For example, a 40-year-old doctor on duty in a hospital in Faridabad was assaulted by attendants of a patient as the doctor was attending to another patient, he could not immediately attend to the patient.
- Brings Deterrence: Allowing unruly behaviour to go unchecked might enable a cycle of disruptive or non-compliant behaviour, which could negatively impact the patient’s overall health outcomes. By refusing treatment, the doctor may communicate that certain standards of behaviour are expected for a therapeutic relationship to proceed.
- Right to Freedom to practise any profession: The regulations give the doctors the right to choose whom they will serve, except in case of a life-threatening emergency.
- Financial Constraints
- Autonomy and Consent: Doctors are ethically obligated to provide patients with accurate information about their treatment options, including potential costs.
- If a patient cannot afford the treatment, the doctor might argue that proceeding with treatment without full financial transparency could undermine the patient’s autonomy and informed consent.
- In extreme cases, relatives of patients have been known to hold doctors or hospital staff hostage, demanding treatment.
- Professional Boundaries: Some proponents of this perspective argue that doctors have a professional duty to provide medical care and expertise, but they are not obligated to address broader societal issues such as patients’ financial difficulties.
- Ethical Boundaries: Doctors have ethical responsibilities not only toward their patients but also toward themselves, their families and the healthcare community.
- For example, potential threats and violence have long-lasting impacts which manifests in the degradation of personal and professional relations.
- Objectivity: Taking decisions which are free from subjectivity caused by emotions, perceptions and individual bias is necessary for long term sustainability.
- For example, Free medical care for a desperate patient may be ethical, but providing it to many patients may not be feasible for one provider.
- Selfless Duty: Medical practitioners often prioritize the well-being of their patients above their own comfort, personal time and space. However, the job can be thankless at times.
- For example, During COVID-19 despite their selfless dedication, medical professionals were subjected to regular assaults and verbal abuse throughout the country.
Arguments against the Regulation
- Dedication and the Duty of Care: Dedication is the sense of deep rooted commitment to devote oneself to a cause.. This includes a duty to provide care to those in need, regardless of their financial status.
|
The Hippocratic Oath
- It is a historic ethical code traditionally taken by medical professionals to uphold certain moral and professional standards in their practice.
- It is named after the ancient Greek physician Hippocrates, who is often referred to as the “Father of Medicine.”
- The exact wording of the oath can vary but the underlying principles remain consistent.
|
-
- In India, out-of-pocket health expenditure accounts for more than half of total health expenditure pushing many households into poverty. This shows the dire need for empathy and compassion towards those in need.For example, Dr Ramanand Singh has been treating his patients for just Rs 50 for the past 35 years in Bihar. He even waives off his fees in cases where the patients cannot afford medical treatment.
- Justice and Equity: The principle of justice requires that healthcare be distributed fairly and equitably. Denying treatment to a patient solely based on their inability to pay could be seen as unjust, perpetuating disparities in healthcare access.
- Hippocratic Oath: Physicians pledge to do what is in the best interest of their patients and to avoid causing harm.
- Physicians promise to treat all patients fairly, regardless of their background, and to provide care to the best of their abilities without bias.
- Unholy Nexuses: Many doctors form nexuses with drugmakers to prescribe specific drugs from their brand instead of generic drugs leads to considerable rise in treatment costs for patients.
- For example, freebies given to doctors including travel expenses, gifts etc. by drugmakers is a common practice.Beneficence: It means kindness or generosity and this principle refers to the moral obligation to act in a manner that will benefit others.The principle of beneficence obligates doctors to act in the best interests of their patients and to promote their well-being.
- Compassion: It is the desire to end someone’s suffering which forms the core principle of a medical practitioner. Refusing treatment to individuals on certain grounds could lead to the possibility of crisis of conscience among several practitioners.
- Loss of Trust and Credibility: The medical profession relies on public trust, and denying treatment to those in need could erode that trust and damage the reputation of the medical community.
- Responsibility: Some argue that healthcare professionals have a broader social responsibility to address systemic issues in healthcare, including affordability and access. Refusing treatment might be seen as abdicating this responsibility.
- Undermining Right to Life: Providing a legal caveat for the registered physicians to refuse treatment is against the fundamental right guaranteed under Article 21 of the Constitution.
- Further, there is no specific definition of “abusive” in law as it is purely a subjective interpretation that may depend on the personal opinion of any individual.
- Subjective interpretation may further lead to exclusion on the basis of race, religion, caste, sex etc.
What Should be Done?
Initiatives towards protection:
- Epidemic Diseases Act 2020: It includes protections for healthcare personnel combatting epidemic diseases and expands the powers of the central government to prevent the spread of such diseases.
- Healthcare Service Personnel and Clinical Establishments (Prohibition of violence and damage to property) Bill, 2019: The draft bill aims to provide protection to healthcare service personnel and clinical establishments against acts of violence and damage to property.
- International Best Practice: The National Health Service in the United Kingdom has implemented measures to protect healthcare workers, including security measures at hospitals and training programs to manage challenging situations.
|
- Persuasion: Influencing patients to follow prescribed norms for behaviour and ensuring smooth functioning.
- For example, during COVID-19 pandemic, voice messages were circulated using caller tune to make people aware of the importance of vaccination and prevent attacks on health workers.
- Emotional Intelligence: Equipping and training medical personnel with necessary skills so that they can manage their emotions and try to avoid escalation of situation and providing practical solutions to the given problems.
- Transparent Approaches: Consider alternative approaches before refusing treatment. This might involve social workers, mental health professionals, or conflict resolution experts to address the underlying issues contributing to the unruly behaviour.
- For example, Doctors in San Diego (USA) refer patients to low-cost family health centers that provide caring, affordable, high-quality health care and supportive services to everyone.
- Ethical Principles Balancing: Weigh the principles of patient autonomy, duty of care, patient safety, and respect for healthcare personnel’s well-being. Consider how refusing treatment aligns with these principles and what potential consequences might arise from the decision.
- For example, Doctors Without Borders is a Nobel Peace Prize receiver charity that provides humanitarian medical care in conflict zones to all those in need of medical care, irrespective of the role played by them in the conflict.
- Tolerance: Accepting actions and practices which may be considered to be incorrect but still tolerable to some extent that they should not be prohibited or penalised heavily.
- For example, a significant number of the cases of unruly behaviour arises in situations which may not be considered as “common” and even the most well-behaved might behave in a way which is not acceptable in society due to the shock or intensity of the moment which one may not be able to handle.
- Consent: Communicating the decision clearly to the patient, and explaining the reasons behind it thus ensuring that the patient understands the potential consequences of their behaviour on their health and the doctor-patient relationship.
- Offering Continuity of Care: If possible, provide recommendations for alternative sources of care, whether within your healthcare institution or elsewhere. Ensure the patient’s ongoing health needs are addressed.
Conclusion
We must protect those who heal. Ethical decisions in healthcare are rarely black and white. It’s important to approach each situation with sensitivity, professionalism, and a commitment to upholding the well-being of patients, healthcare staff, and the broader community. Consulting with colleagues, supervisors, and ethics committees can provide valuable guidance in making these difficult decisions.
News Source: The Hindu
![]() 25 Aug 2023
25 Aug 2023