Researchers have developed a groundbreaking in vivo CAR-T cell therapy that reprograms immune cells directly inside the body using mRNA, eliminating the need for lab-based manipulation known as In vivo CAR T-cell generation
How does In vivo CAR T-cell generation work?
- Researchers engineered CAR T-cells directly in the body using mRNA + lipid nanoparticles (LNPs).
| Cytotoxic T cells are also called CD8+ cells because they have a CD8 receptor on their membranes. Cytotoxic T cells kill cells infected with viruses and bacteria, and they also destroy tumor cells. |
- LNPs carry mRNA with CAR instructions and are targeted to CD8+ T cells using specific antibodies.
- Once infused into bloodstream:
- T cells absorb mRNA
- Temporarily express CAR
- Seek & destroy target B cells (e.g. CD19+, CD20+)
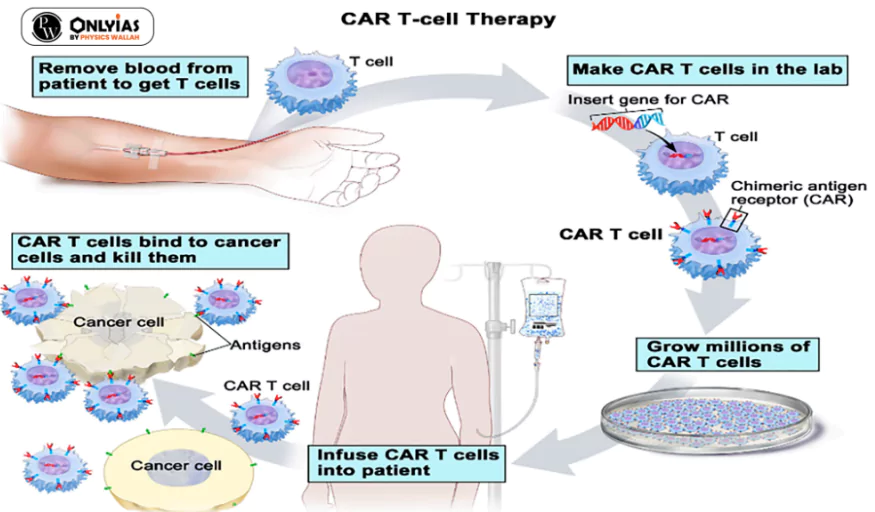
What is CAR-T cell therapy?
- CAR T Cell is a novel and highly complex immune therapy that redirects the body’s immune system to fight cancer.
| T-cells are a type of white blood cell (lymphocyte) that play a central role in the immune system. Their primary function is cytotoxic — they identify and kill abnormal cells, including virus-infected or cancerous cells. |
- CAR-T cells are often described as ‘the living drug’ because they actively search and target malignant cells.
- Principle: It uses a type of immune cell called a T-cell, which is extracted from a patient’s blood before being genetically altered to allow it to target surface proteins found on cancer cells.
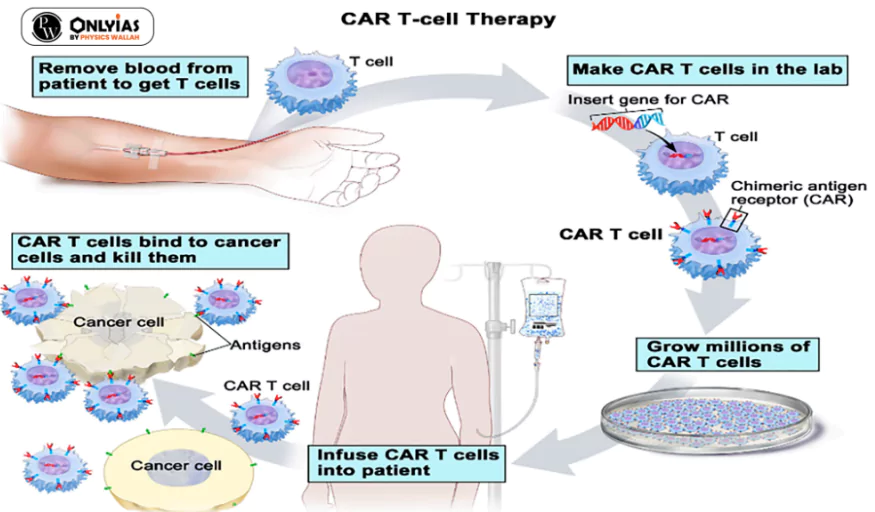 Mechanism: The patient’s T-cells (types of immune cells) are collected and genetically modified into potent cancer fighters known as CAR-T cells.
Mechanism: The patient’s T-cells (types of immune cells) are collected and genetically modified into potent cancer fighters known as CAR-T cells. - The genetically modified cells express chimeric antigen receptors (CARs) specific to cancer cells.
- The modified CAR-T cells are then expanded in the laboratory before being infused into the patient.
- Once in the body, these engineered cells recognise and attack cancer cells, with a focus on B-cell cancers, thus offering a targeted and potent immunotherapy.
Why is CAR T Cell therapy effective?
- Improves immunogenic memory, which provides continuous surveillance to treat local and distant metastatic lesions.
- Recognises and eliminates damaged cells and cells infected with harmful pathogens, such as viruses and cancerous cells.
- Reduces the need for aggressive chemotherapy and Bone transplantation.
- Affordability: Indigenous CAR-T cell therapy brings treatment costs down from Rs 4 crore to Rs 40 lakh.
- Success Rate: In studies, 9 out of 10 people with acute lymphoblastic leukemia whose cancer didn’t respond to other treatments or whose cancer came back had complete remission with CAR T cell therapy.
- Remission means the cancer can’t be detected in tests.
Significance of in vivo CAR-T cell therapy
- Conventional CAR T (India): ₹60–70 lakh (~₹30–35 lakh for cell processing)
- New method advantages:
- No specialised cell manufacturing — reduces cost and complexity
- Avoids chemo-based lymphodepletion — lowers infection risk, shortens hospital stay
- Safer for frail, elderly, or comorbid patients.
- India has high incidence of B-cell driven cancers like:
- Diffuse large B-cell lymphoma (34–60% of non-Hodgkin lymphoma)
- Acute lymphoblastic leukemia (75% of childhood cancers)
Limitation
- Still preclinical — human trials pending.
![]() 25 Jun 2025
25 Jun 2025

 Mechanism: The patient’s T-cells (types of immune cells) are collected and genetically modified into potent cancer fighters known as CAR-T cells.
Mechanism: The patient’s T-cells (types of immune cells) are collected and genetically modified into potent cancer fighters known as CAR-T cells. 