Context
World TB Day is celebrated annually on 24 March to raise awareness about the tuberculosis disease.
World TB Day 2024
- World TB Day commemorates the discovery of Mycobacterium tuberculosis.
- Discovered by: On 24 March 1882, Dr. Robert Koch announced the discovery of the bacteria that causes tuberculosis (TB).
- World TB Day 2024 Theme: ‘Yes, we can end TB!’
About Tuberculosis (TB):
- An Infectious Disease: Tuberculosis (TB) is an infectious disease that most often affects the lungs and is caused by bacteria, Mycobacterium tuberculosis.
- Transmission: It spreads through the air when infected people cough, sneeze or spit.
- About 5–10% of people infected with TB will eventually get symptoms and develop TB disease and those who are infected but not (yet) ill with the disease cannot transmit it.
- Prevention: TB is preventable and curable.
- It is usually treated with antibiotics and can be fatal without treatment.
- The most common antibiotics used are: isoniazid, rifampin, pyrazinamide, ethambutol and streptomycin.
- In certain countries, the Bacille Calmette-Guérin (BCG) vaccine is given to babies or small children to prevent TB, which prevents TB outside of the lungs but not in the lungs.
- Existing Forms: The disease exists in both latent and active form.
- Latent Form: The latent type does not express any symptoms and is not transmissible unless it develops into the active type.
- Active Form: This form expresses symptoms such as chronic cough and bloody mucus.
- Antibiotics are typically administered for a minimum of six months, and ensuring the course is completed is vital to prevent antibiotic resistance.
Tuberculosis- A Concerning Disease & Statistics
- A Global Pandemic: As per the World Health Organisation (WHO), TB remains a global pandemic, with 1.8 billion people estimated to be infected.
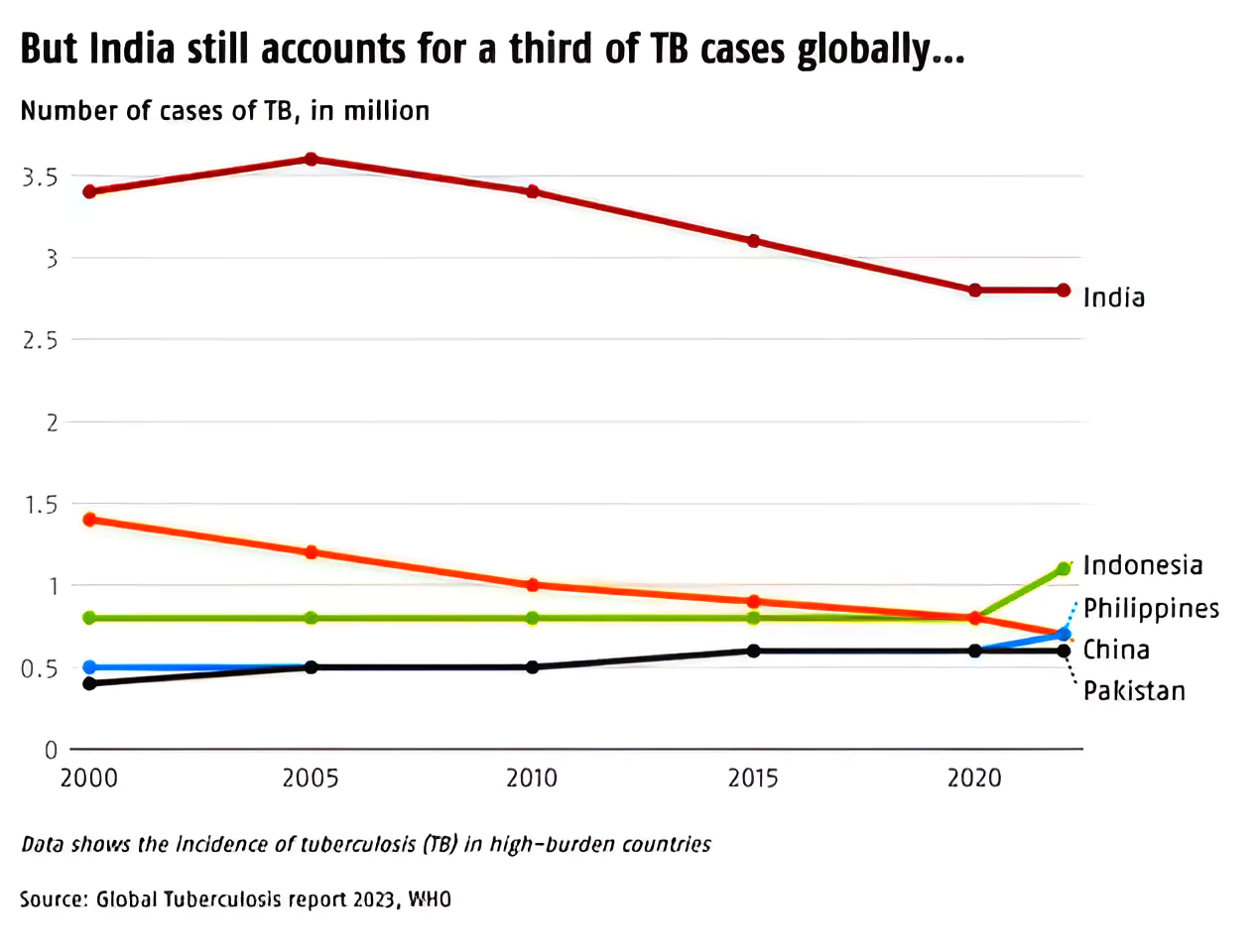
- Top eight high-burden countries included India, Indonesia, China, the Philippines, Pakistan, Nigeria, Bangladesh, and the Democratic Republic of Congo.
- Medically, the greatest challenge is posed by the multi-drug resistant (MDR) variant of the disease.
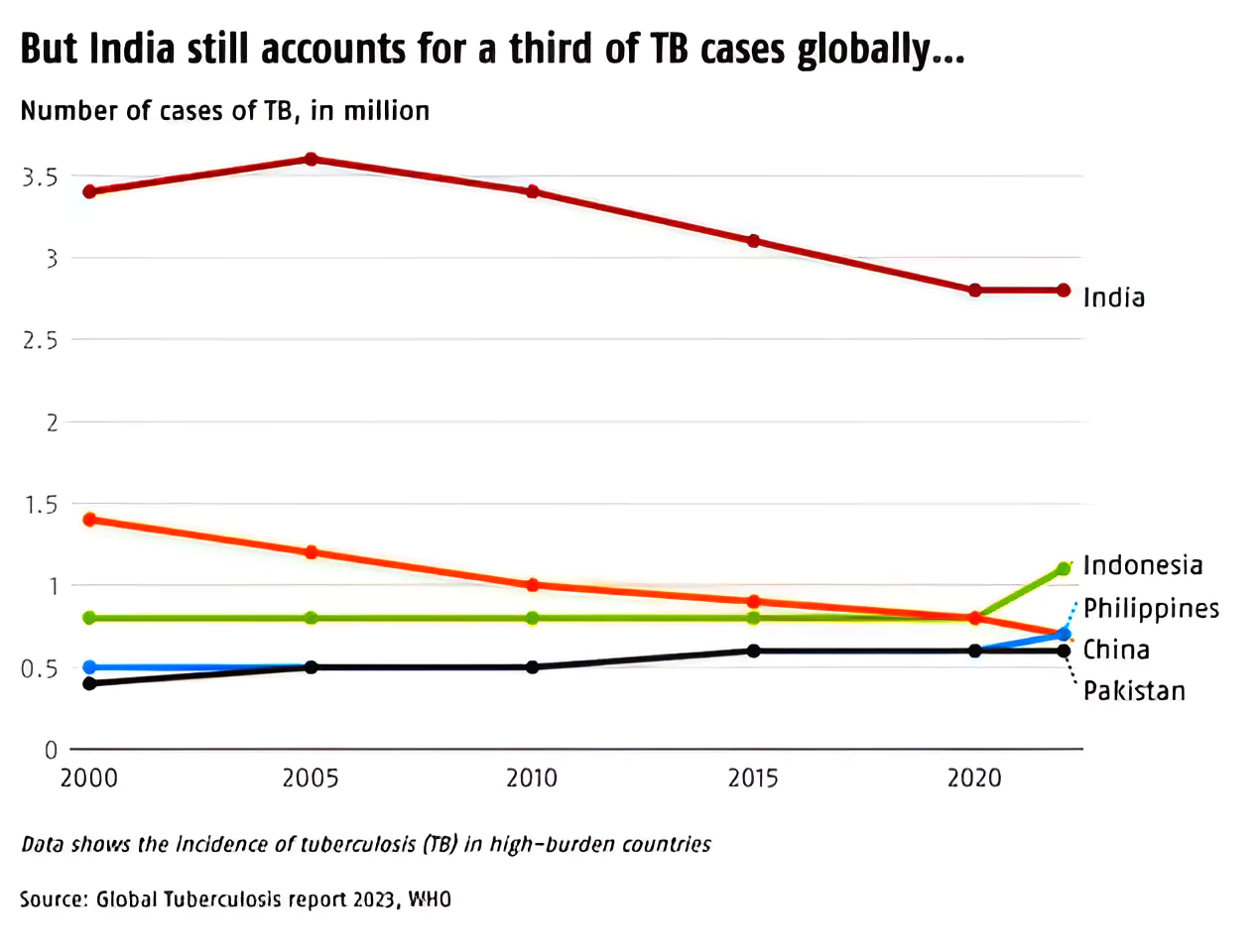
- India’s Position: As per Global TB Report 2023 (released by the WHO), India has the highest incidence of bacterial infection and accounts for 27% of the total TB cases in the world.
- In 2022, India reported 2.8 mn TB cases, meaning one person gets TB every 11 seconds.
- The WHO estimated that 1,19,000 new cases of MDR TB emerge in India each year.
- High Mortality Rate: Without treatment, the mortality rate is high, at about 50%.
 However, with treatments, recommended by WHO, about 85% of TB patients can be cured.
However, with treatments, recommended by WHO, about 85% of TB patients can be cured.
- Drug-Resistant TB: Tuberculosis that does not respond to standard drugs is called drug-resistant TB and requires more toxic treatment with different medicines.
- Types: It has two main types:
- Multidrug-Resistant Tuberculosis (MDR-TB): It is a form of TB caused by bacteria that do not respond to at least isoniazid and rifampicin, the two of the most effective TB drugs.
- MDR-TB is treatable and curable by using second-line drugs such as Bedaquiline (practically incurable by standard first-line treatment).
- Extensively Drug-Resistant TB (XDR-TB): It is a more serious form of MDR-TB caused by bacteria that do not respond to the most effective second-line anti-TB drugs, often leaving patients without any further treatment options.
How Does Drug Resistance Happen?
- Resistance to anti-TB drugs can occur when these drugs are misused or mismanaged.
- Examples: Patients do not complete their full course of treatment; health-care providers prescribe the wrong treatment, the wrong dose, or length of time for taking the drugs; the supply of drugs is not always available; or the drugs are of poor quality, etc.
|
Global Actions to Eradicate Tuberculosis
-
End TB Strategy By WHO:
- It serves as a blueprint for countries to reduce TB incidence by 80%, TB deaths by 90%, and to eliminate catastrophic costs for TB-affected households by 2030.
- The WHO has launched a joint initiative “Find. Treat. All. #EndTB” with the Global Fund and Stop TB Partnership.
- WHO releases the Global Tuberculosis Report.
- WHO also published the World Development Report (1993), which labeled TB treatment for adults as the best buy among all developmental interventions.
-
The Global Fund:
-
- It is a private public partnership aimed at leveraging and providing funding for HIV, TB and malaria and ensuring a healthier, safer, more equitable future for all.

-
The Stop TB Partnership:
- It was established in 2001 to eliminate tuberculosis as a public health problem. Its 2000 partner organizations include international, non-governmental and governmental organizations and patient groups.
- The 2023-2028 Operational Strategy exists to provide a living, high-level roadmap for current and future work of the Secretariat, bringing the organization together around its comparative advantages and achieving greater sustainability.
-
Sustainable Development Goal (SDG) 3:
- To end the TB epidemic by 2030.
- Goal 3.3: By 2030, end the epidemics of AIDS, TB, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.
- India is a signatory of the United Nations SDGs and has targeted TB elimination by 2025, five years ahead of the SDG timeline.
India’s Efforts to Eradicate Tuberculosis
- National TB Programme (NTP): The Government of India launched NTP in 1962 as District TB Centre model involving imparting BCG vaccination and TB treatment to fight tuberculosis.
- The National Tuberculosis Elimination Programme (NTEP): It was launched in 2017 by the Ministry of Health and Family Welfare (MoHFW).
- It sets out how the government proposed to eliminate TB in India describing the activities and interventions that would bring about major and effective changes in the incidence, prevalence and mortality from tuberculosis
- The National Strategic Plan (NSP) for TB Elimination: The NSP for TB Elimination 2017–25 is a bold strategic framework to drive the acceleration of progress toward TB Elimination, achieving the SDGs and the End TB targets for India. It adopts strategies under four pillars- Detect, Treat, Prevent and Build.
- Nikshay TB Program: Nikshay is a TB control programme, to monitor and track services and status related to screening, diagnosis, treatment and follow-up of TB cases. Alerts to TB patients regarding medication, follow-up alerts to the patients and providers etc.
- Nikshay Poshan Yojana (NPY): The NPY was launched in 2018 by the MoHFW with an aim to support every TB patient by providing a Direct Benefit Transfer of Rs 500 per month for nutritional needs.
- Nikshay Mitra: In September 2022, India launched another nutrition support programme called Ni-kshay Mitra to consented TB patients.
- Patient Provider Support Agencies (PPSA): PPSA is a model under which a third-party agency/non-governmental organization is selected by a state/city/district NTEP unit to engage private-sector doctors treating persons affected by TB to provide end-to-end services, such as diagnosis, notification, patient adherence and support, and treatment linkages.
- Universal Drug Susceptibility Testing (UDST) – To ensure every diagnosed TB patient is tested to rule out drug resistance before or at the time of treatment initiation itself.
- Pradhan Mantri TB Mukt Bharat Abhiyaan (PMTBMBA): It is an initiative of the MoHFW to accelerate India’s progress towards TB elimination by 2025 by bringing together all community stakeholders.
- NIKSHAY 2.0 Portal: For effective implementation of PMTBMBA initiative, the Ni-kshay 2.0 portal provides a platform for community support to TB patients and is accessible in the public domain.
- Ayushman Bharat- Health and Wellness Centres: To decentralize the comprehensive primary healthcare including TB care services at the grassroots level.
- The Saksham Project: It is a project of the Tata Institute of Social Sciences (TISS) that has been providing psycho-social counselling to TB patients.
- It focuses on supporting and strengthening national response for both HIV and TB without creating parallel structures.
Achievement By India
- Decline in TB Incidence and Mortality: As per the Global TB Report 2023, since 2015, TB incidence and mortality in India have declined by 16% and 18% respectively, faster than the decline globally.
- Supporting Factors:
-
- The role of programmes like NTEP and PM-Nikshay are helping in reducing incidence and mortality rates.
- Various initiatives focus on early diagnosis, ensuring complete treatment, and providing nutritional support and has contributed to higher cure rates and reduced TB spread.
- Accessibility of TB drugs in India.
- All first-line TB drugs are now accessible even in remote areas.
- Costly medicines like bedaquiline are available in government institutions, aiding in curing many cases of MDR-TB.
|
Addressing India’s Tuberculosis Eradication Challenges
-
Time Constraint for 2025 Target:
- In its 149th report in Parliament, the Department-related Parliamentary Standing Committee on Health and Family Welfare said the task at hand is enormous and time is short to meet the End TB target by 2025.
-
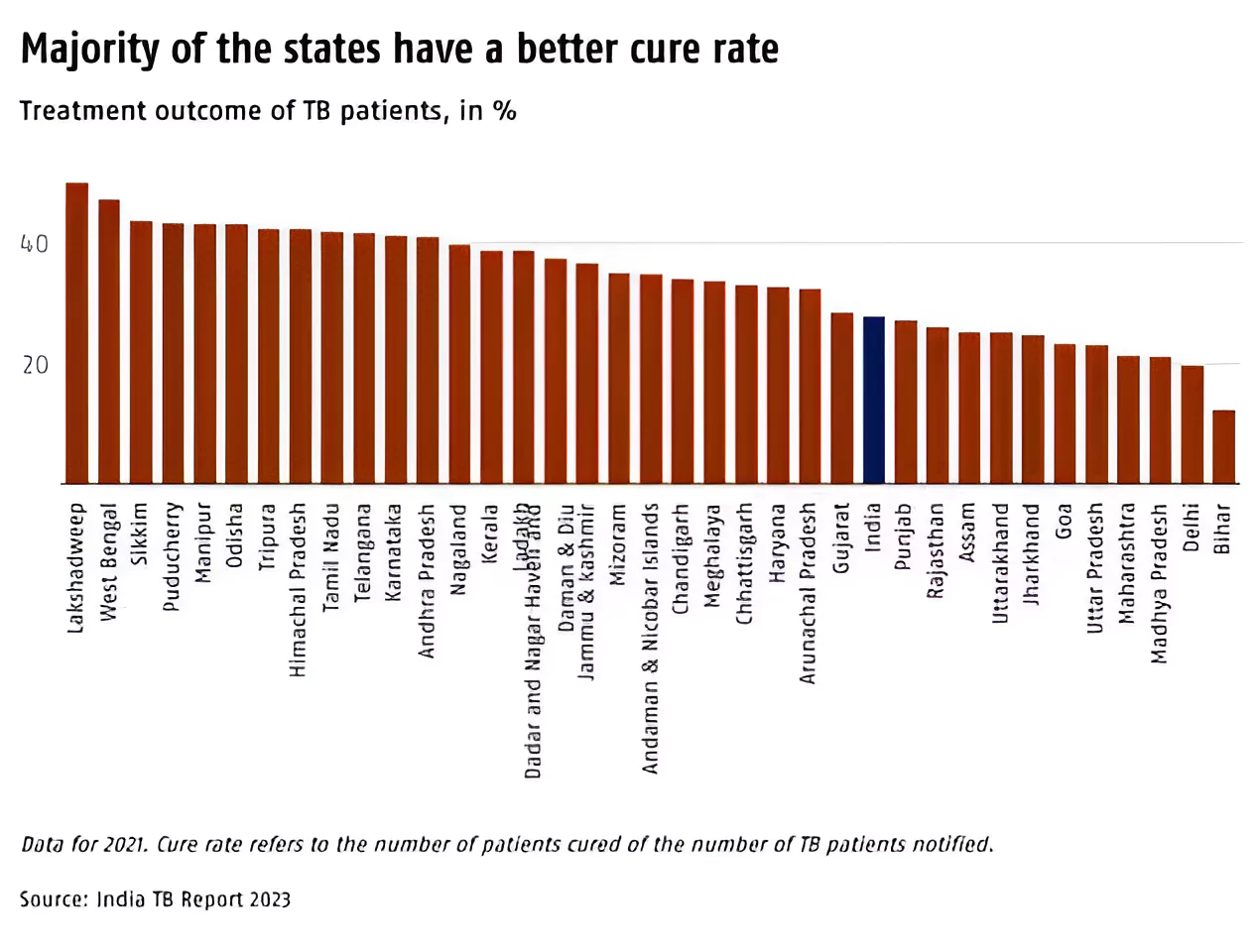
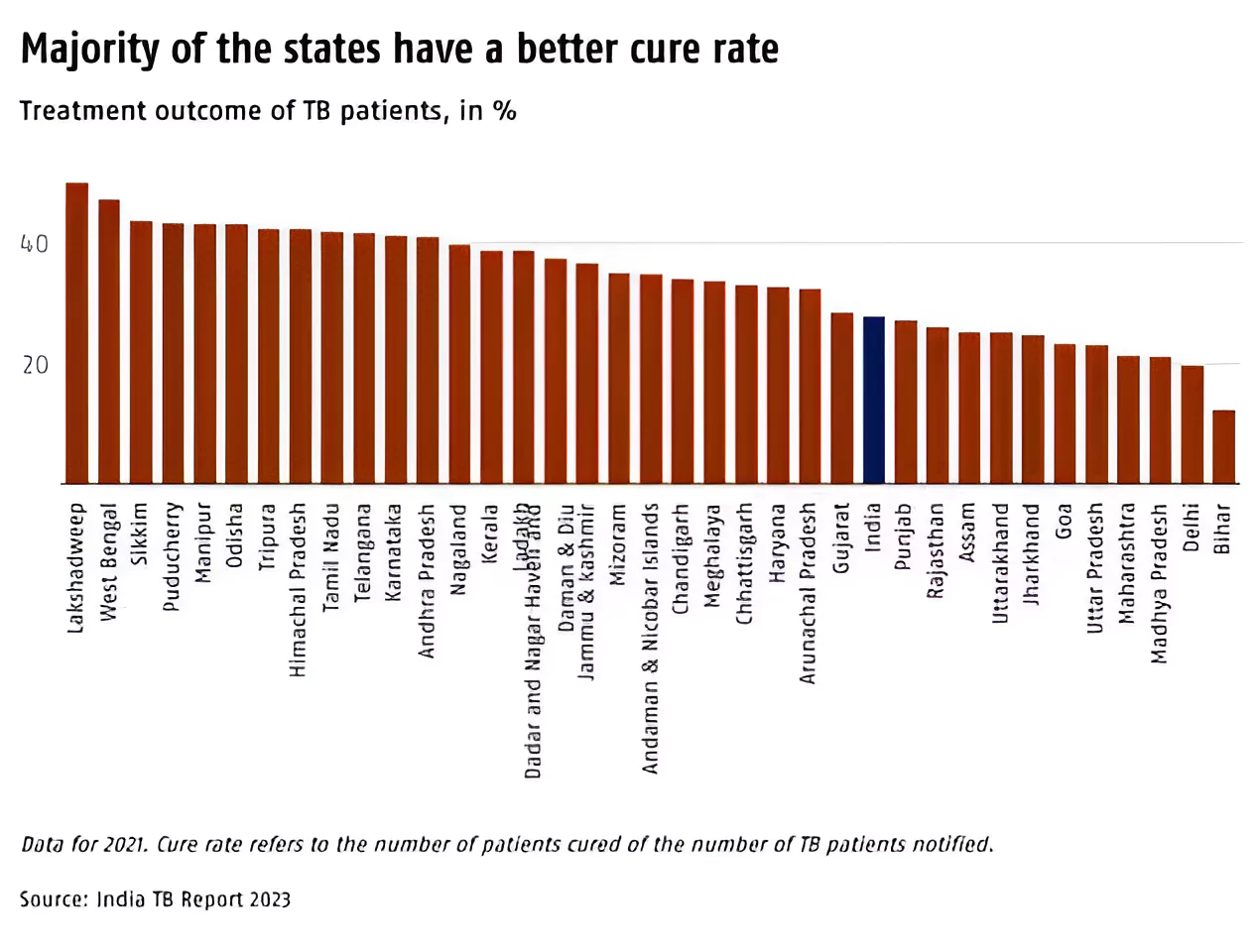
Regional Differences in TB Cure Rate in India:
-
- With India’s 2025 deadline to end TB drawing near, some states are lagging behind others. While India’s TB cure rate stands at 27.8%, 11 states have rates lower than the national average.
- Lowest Cure Rate: Bihar, Madhya Pradesh, Uttar Pradesh and Rajasthan. Goa and Maharashtra also exhibit low cure rates.
- The majority of patients reside in the Bimaru (acronym for Bihar, Madhya Pradesh, Rajasthan, and Uttar Pradesh) states.
- Together, the Bimaru states account for two-thirds of the population in states with cure rates below the national average.
| Bimaru: It was coined in the 1980s, to refer to states lagging in key economic and other indicators, including the availability of health services needed to address diseases like TB. |
-
Poverty:
- It is one of the big problems of undernourishment and poor and unhygienic living conditions and the majority of TB patients in India are due to undernourishment.
- As per the Health Ministry, undernutrition contributes to 55% of annual TB incidence in India.
- A 2022 study noted that 45% of people in India are undernourished, accounting for nearly 1.2 million TB cases each year.
-
Underreporting:
- One of the major factors of TB prevalence in India is under-reporting which escalates the risk of spread of TB to other healthy individuals.
- According to the target set by NSP, in 2022, there should have been 1.93 million TB notifications by the private sector. Yet, there were only 0.73 million notifications. A staggering 1.2 million TB cases in the private sector were missed in 2022.
-
Inadequate Diagnosis:
- Biomarkers and other diagnostics that identify individuals at highest risk of progression to disease are inadequate.
- Also, doctors in India are less and untrained to diagnose and cure the disease.
-
Missing in Treatment:
- Inequitable access to quality diagnosis and treatment is a major issue.
- As per a report by a National Institute of Epidemiology team, the national level, 9.3% of the population were screened, just 1% of the screened were tested and 3.7% of the tested were diagnosed.
-
Drug Resistant TB:
- Standard TB treatment is not followed uniformly across the private sector, resulting in the rise of drug resistance and results in MDR-TB and XDR-TB.
- Over a quarter of Indian patients carry TB bacteria that are resistant to at least one anti-TB medication.
-
Social Stigma:
- Patients often hesitate to seek treatment or deny due to fear of social discrimination and stigmatisation.
-
Challenge with People with Disabilities:
- A person with a disability finds it challenging to visit the health facility every month to collect medicines or meet the doctor.
- Disability is as yet not recorded in the post-treatment follow up protocol, leading to data gaps in estimating the scale of the problem.
-
Miscellaneous:
-
- Human resource shortage, payment delays, procurement delays, drug stock-outs etc., are other concerning challenges.
Way Forward to Tuberculosis – Eradication & Prevention
-
Prevention and Early Diagnosis:
- These are key to stopping the ongoing spread of the disease. Continuous monitoring for identification of adverse TB drug reactions must be strengthened.
- Within a district, all high-risk populations are to be first identified (called as mapping) and active case finding should be conducted among them.
-
Vaccines Development:
- There is a need for updated and improved prophylactic vaccines. By investing in developing better vaccines, ultimate elimination of TB is possible.
- The prophylactic use of vaccines has a very low risk of generating resistance.
-
Convergence of Policy Initiatives is Essential:
- Increased investment, improved awareness, and adoption of WHO recommendations are essential to reduce the burden of TB over time.
- Urgent action is required to end the global TB epidemic by 2030, a goal that has been adopted by all Member States of the United Nations (UN) and the WHO.
- Universal Health Coverage (UHC) is essential to ensure that all people who need treatment for TB disease or infection can access these treatments.
-
A Comprehensive Solution:
- Customised, person-centred care and support takes into account for disabled persons’ unique needs and post-treatment protocols must extend to providing access to comprehensive support services.
-
Reduce Stigma & Support Empowerment:
- By supporting frontline TB workers, strengthening supply chains and procurement mechanisms, decentralising TB services and empowering local communities can reduce stigma and enhance treatment outcomes.
-
Need For a Multi-Sectoral Approach:
-
- Poverty alleviation, improvement in nutritional status, well-ventilated housing and better air quality will all contribute towards reducing TB.
-
- Leveraging technology and innovation holds promise in enhancing TB care efforts. The adoption of AI and digital health solutions for TB diagnosis, adherence and surveillance can revolutionise the way TB care is delivered and accessed.
-
Person-Centred Solutions:
-
- The needs and the interests of patients and communities must be prioritized within the care paradigm and the health- care system.
- This principle, echoed by survivors, communities, health experts and policymakers, underscores the need for a person-centred approach to TB care and management.
Conclusion
The path to TB elimination requires a concerted effort to prioritise person-centred care, address social determinants of health, and embrace innovation. By adopting a holistic and person-centred approach, India can overcome the barriers and create a healthier future for all its citizens.
Also Read: Role Of X Chromosome In Autoimmune Diseases
![]() 26 Mar 2024
26 Mar 2024
 However, with treatments, recommended by WHO, about 85% of TB patients can be cured.
However, with treatments, recommended by WHO, about 85% of TB patients can be cured.