World Organ Donation Day, observed annually on 13 August, serves as a global reminder of the life-saving potential of organ and tissue donation.
About the World Organ Donation Day
- An annual event observed to raise awareness about the life-saving power of organ donation and to honour donors and their families for their selfless contributions.
- Objective: Raise awareness about organ and tissue donation, dispel myths, and encourage voluntary pledging.
- Theme 2025: “Answering the Call”, highlighting both individual pledges and systemic readiness.
History of World Organ Donation
- First Successful Transplant: The history of organ transplantation began with the world’s first successful organ transplant on December 23, 1954.
- Pioneer Donor: Ronald Lee Herrick was the first living organ donor, giving a kidney to his twin brother, Richard Herrick.
- Nobel Prize Winner: The transplant was performed by Dr. Joseph Murray, who received the Nobel Prize in Physiology or Medicine in 1990 for his groundbreaking work in organ transplantation.
- Establishment of the Day: World Organ Donation Day was first observed in the early 2000s to promote the idea of organ donation.
- Founding Organizations: The initiative was led by organizations such as the World Health Organization (WHO) and the International Society for Organ Donation (ISOD).
About Organ Donation
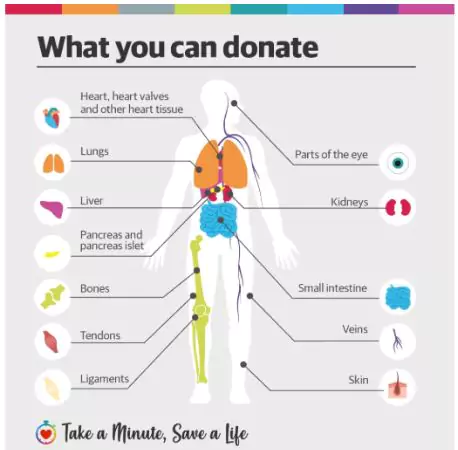
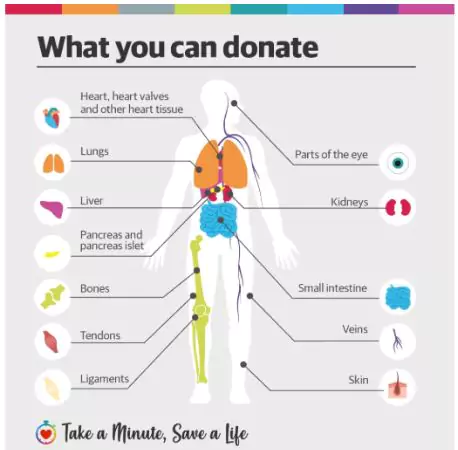
- Refers: Organ donation involves transplanting healthy organs (e.g., kidneys, heart, liver) or tissues (e.g., corneas, skin) from living or deceased donors to patients with organ failure.
- Organs that can be donated include the heart, kidneys, liver, lungs, and pancreas.
- Tissues that can be donated include corneas, skin, and bone marrow.
- Types of Organ Donation:
- Living Donation: A living person donates an organ, such as a kidney or a portion of their liver.
- Deceased Donation: Organs are donated after a person has been declared brain dead or has suffered cardiac death.
- Eligibility for Organ Donations in India:
- Living Donors:
- Age: Generally, individuals aged 18 to 65 are considered eligible.
- Health Status: Must be in good health, free from diseases like active cancer, infections, or uncontrolled diabetes.
- Relationship: For kidney and liver donations, the donor should typically be a near relative (parent, sibling, child, grandparent). Donations from unrelated individuals are permissible but require rigorous scrutiny and approval by a Transplant Authorization Committee.
- Deceased Donors:
- Brain Death: Organ donation after death is permissible only if the individual has been declared brain dead by a medical board in a hospital.
- Age Limit: The previous upper age limit of 65 years for receiving organs has been removed; individuals of any age can now register to receive a deceased donor organ.
|
List of Organs that can be Donated
|
| Kidneys |
- Most commonly transplanted organ; can be donated by living donors
|
| Heart |
- Vital organs, often donated after brain death
|
| Liver |
- Can regenerate; parts can be donated by living donors
|
| Lungs |
- Donated as a pair or single lung, often for patients with respiratory diseases
|
| Pancreas |
- Helps patients with severe diabetes
|
| Intestines |
- Less common but life-saving in critical digestive disorders
|
| Tissues |
- Corneas, skin, bones, tendons, improves quality of life for recipients
|
- Current Scenario:
- Global Demand: Over 1,06,000 people worldwide await life-saving transplants (UNOS data).
- India’s Waiting List: About 63,000 for kidney transplants, and about 22,000 for liver transplants.
- India’s Progress: In 2024, over 18,900 transplants performed (highest ever), ranking 3rd globally after US & China.
- India is the leader in hand transplants worldwide.
- State-wise: Telangana tops the country in the number of deceased donors, Tamil Nadu and Karnataka.
- Gaps Existing: Lakhs require transplants annually, but only a fraction receive them due to low awareness and system inefficiencies.
- Historical Evolution of Organ Transplantation in India:
- Pre-1994: Donations were primarily from living relatives, with no legal recognition of brain death, leading to rampant organ trade in the 1980s–90s.
- 1994: The Transplantation of Human Organs Act (THOA) recognized brain death, banned commercial organ trade, and established ethical oversight through authorization committees.
- 2000s–2010s: The National Organ and Tissue Transplant Organisation (NOTTO), established in 2014, along with Regional (ROTTOs) and State (SOTTOs) bodies, streamlined operations. Green Corridors facilitated rapid organ transport.
- Green Corridors are special routes that enable fast, uninterrupted transport of organs, preserving viability and saving lives.
- 2020s: Digital pledging portals and integration with Aadhaar and digital health IDs enhanced donor-recipient matching.
| PWOnlyIAS Extra Edge:
Case Study – Riya’s Gift of Life:
- Background: Riya, a 21-year-old engineering student, suffered a fatal road accident in Pune. She had pledged her organs at age 18 after attending a college awareness session.
- Consent & Coordination: Her family was aware of her wishes and readily consented to donation.
- The Zonal Transplant Coordination Centre initiated the process within 3 hours of hospital confirmation of brain death.
- Impact: This gave a new life to five others:
- Heart: Saved a 12-year-old boy with congenital heart disease.
- Kidneys: Transplanted into two patients on the waiting list for over 3 years.
- Corneas: Restored sight to two individuals.
- Ethical Significance:
- Demonstrating respect for autonomy, the family honoured Riya’s recorded decision.
- Showcases empathy and social responsibility in action.
- Highlights the role of awareness programmes in motivating youth.
|
Significance of Organ Donation
- Life-Saving Potential: A single deceased donor can save up to eight lives and improve many more through tissue donation.
- Reducing Waiting Lists: Globally, 1.5 million people are on transplant waiting lists, with 5 lakh in India alone, underscoring the urgent need for donors.
- Example: Tamil Nadu’s cadaver programme reduced kidney transplant wait times by nearly 40% in some districts.
- Promoting Altruism: Donation fosters a culture of generosity, offering emotional closure to donor families.
- Example: The family of a 16-year-old accident victim in Pune donated her organs in 2024, benefiting seven critically ill patients across Maharashtra.
- Healthcare Equity: Public funding and inclusive policies ensure access transcends economic and social barriers.
- Example: Under Kerala’s scheme, 50% of state-funded cadaver kidney transplants go to patients from Below Poverty Line (BPL) families.
- Medical Advancement: Ethical transplant systems counter organ trade and drive innovation in medical technology.
- Example: In 2025, Chandigarh PGIMER performed India’s first successful robotic-assisted kidney transplant from a living donor, reducing recovery time by 30%.
| PWOnlyIAS Extra Edge:
The Organ Donation Process in India:
- When a Potential Donor Passes Away?
- If the deceased has not registered as a donor, the family can still authorise donation by signing a consent form.
- Once consent is given, the transplant coordination team retrieves the organs within hours.
- The body is reconstructed and returned to the family with dignity.
- Disfigurement & Funeral Concerns:
- No disfigurement: As AIIMS clarifies, organ retrieval is surgical and respectful; the body can be viewed normally.
- No delay: Funerals proceed as scheduled.
- Why Pledging is Important?
- Ensures your wishes are officially recorded.
- Reduces emotional stress for family members during grief.
- Speeds up organ retrieval, improving transplant success rates.
About National Organ and Tissue Transplantation Organisation (NOTTO):
- It is a National level apex organization set up under the Directorate General of Health Services, Ministry of Health and Family Welfare in 2014.
- Objective: To facilitate coordination and networking in organ transplantation activities.
- Function and Responsibilities:
-
- Lay down policy guidelines and protocols.
- Compile and publish registry data.
- Maintaining the waiting list of terminally ill patients requiring transplants.
- Consultancy support on the legal and non-legal aspects of donation and transplantation.
|
Challenges with India’s Organ Donation System
- Low Awareness: Myths about body disfigurement deter donations, particularly in rural areas.
- Example: In a 2023 Karnataka study, over 60% of respondents believed organ donation disfigures the body, despite medical clarification that retrieval is performed with surgical dignity.
- Infrastructure Gaps: Shortages of ICU beds, trained coordinators, and organ preservation facilities.
- Example: According to NOTTO’s 2024 Annual Report, only 300 of India’s 1,600 registered hospitals are adequately equipped for multi-organ retrieval.
- Bureaucratic Delays: Slow brain-death certification, especially in smaller hospitals.
- Example: A 2024 audit by TRANSTAN found an average 6–8 hour delay in brain-death declaration in Tier-2 cities, often leading to organ non-viability.
- Financial Barriers: High costs of post-transplant immunosuppressive therapy.
- Example: NITI Aayog’s 2023 review flagged that over 40% of kidney transplant recipients discontinue or underdose medication within 2 years due to cost.
- Geographic Disparity: Transplant centers are concentrated in southern and western India.
- Example: Tamil Nadu and Maharashtra account for over 50% of India’s deceased organ donations, while states like Bihar and Nagaland reported zero cadaver donations in 2024.
- Low Deceased Donor Rate: India’s rate is ~1 per million population, compared to Spain’s 30–50, with 2 lakh viable organs wasted annually due to under-detection and logistical delays.
- Example: As per AIIMS study, 2024 nearly 2 lakh viable organs are wasted annually due to under-detection of brain death and logistical bottlenecks in transport.
- Gender Disparity in Organ Transplantation: In India, women donate disproportionately more organs but receive far fewer transplants.
- In 2023, women made up 63% of living donors (36,038 of 56,509 over five years), yet account for only 24–47% of recipients across organ types, revealing a profound inequity, for every ten women donors, only four to five women receive transplants.
|
Initiatives and Actions on Organ Donation
|
| India’s Initiatives and Actions on Organ Donation |
- Legal & Policy Framework:
- Transplantation of Human Organs and Tissues Act (THOTA), 1994: The first comprehensive legislation regulating removal, storage, and transplantation of human organs, introducing the legal definition of brain death.
- Brain death is the irreversible cessation of all functions of the brain, including the brainstem, even if the heart continues to beat with the help of a ventilator.
- THOTA (Amendment), 2011: Included human tissues, tightened penalties for illegal trade, and made hospital registration mandatory for transplants.
- THOTA Rules, 2014: Streamlined brain death certification procedures, uniform consent protocols, and fair organ allocation norms.
- Institutional Mechanisms:
- National Organ and Tissue Transplant Organization (NOTTO) – Apex body for national registry management, policy guidance, allocation coordination, and public awareness.
- Regional Organ and Tissue Transplant Organizations (ROTTOs) – Act as zonal coordinators for inter-state organ sharing.
- State Organ and Tissue Transplant Organizations (SOTTOs) – Manage state-level donor-recipient matching, and coordinate with hospitals.
- Digital Platforms & Registries:
- Aadhaar-linked Online Pledge Portal (launched 2023) – Over 3.3 lakh citizens pledged their organs within two years.
- National Waitlist Registry – Real-time list of patients awaiting transplants to ensure transparency.
- Green Corridors – Priority traffic and air routes for rapid inter-city transport of organs, reducing ischemia time.
- Awareness Campaigns:
- Angdaan – Jeevan Sanjeevani Abhiyan – Nationwide campaign with pledge kiosks, webinars, and school outreach.
- National Organ Donation Day (13 August) – Honors donors and spreads public awareness.
- Financial & Logistical Support:
- Rashtriya Arogya Nidhi – Up to ₹15 lakh for poor patients’ transplant costs; ₹10,000/month post-transplant for medicines.
- Ayushman Bharat – PM-JAY – Includes kidney transplant packages under government coverage.
- Best Practice Models in India:
- Tamil Nadu: Cadaver Transplant Program with transparent, equitable allocation, mandatory brain-death certification, TRANSTAN registry, and public-private partnerships for ICU-based organ retrieval.
- Andhra Pradesh: Jeevandan program with mobile coordinators and donor-family counseling.
- Telangana: India’s highest deceased donation rate due to robust hospital coordination.
- Kerala: State-wide network integrating awareness drives with hospital readiness.
|
| Global Initiatives and Actions |
- WHO Guiding Principles on Human Cell, Tissue and Organ Transplantation (2010) – Ethical framework ensuring consent, equity, and non-commercialization.
- Madrid Resolution (2010) – WHO-led global commitment to expand deceased donor programs and ensure ethical practices.
- International Registry in Organ Donation and Transplantation (IRODaT): Global repository of donation and transplant data for monitoring trends.
- Declaration of Istanbul Custodian Group: Promotes ethical donation and fights organ trafficking through global consensus.
|
| Technological & Process Innovations |
- Organ Care Systems (OCS): Portable devices that keep hearts, lungs, and other organs viable longer (“heart in a box” technology).
- Paired Kidney Exchange Programs: Allow incompatible donor-recipient pairs to swap donors through national matching systems (US, South Korea, Netherlands).
- Digital Donor Cards Linked to Health IDs: Used widely in Europe and Canada for quick consent verification.
|
Way Forward
- Awareness Campaigns: Deploy local influencers, religious leaders, and school curricula to dispel myths, especially in rural areas.
- Policy Refinements: Mandate brain-death audits for all ICU deaths, subsidize post-transplant medicines under Ayushman Bharat, and clarify NOTTO’s gender-priority rules to balance equity and medical urgency.
- Infrastructure Expansion: Set up transplant-capable public hospitals in underserved districts, not just metros.
- Digital Integration: Link ICU databases with donor registries for real-time organ matching and use GPS-enabled green corridors for faster transport.
- International Collaboration: Partner with global registries for rare matches and share best practices through WHO and regional health networks.
| PWOnlyIAS Extra Edge:
Lessons for Developing Nations:
- Legislative & Regulatory Strengthening: Recognize brain death in legal frameworks, ban organ trade, and mandate oversight committees in all transplant hospitals.
- Example: India’s Transplantation of Human Organs and Tissues Act (THOTA) is a model, with clear definitions and penalties for violations.
- Robust Institutional Framework: Establish central coordinating bodies like NOTTO, supported by regional and state networks for organ allocation and data management.
- Capacity Building in Healthcare Systems: Train ICU teams, anesthetists, and transplant coordinators to identify and counsel potential donor families.
- Example: Spain’s model — “transplant coordinators in every ICU” — shows a direct link to high donation rates.
- Public-Private & Civil Society Partnerships: Leverage NGOs, CSR funds, and volunteer networks for awareness drives, donor registration, and logistical support.
- Example: MOHAN Foundation in India has registered over 10 lakh pledges through outreach in schools and workplaces.
- Recognition Culture: Publicly honor donor families through state awards, memorial events, and media features to normalize organ donation socially.
- Phased Implementation via Pilots: Begin with regional pilot projects in high-readiness states before national scale-up, ensuring lessons feed into broader rollouts.
|
Conclusion
World Organ Donation Day reaffirms the right to life (Article 21) and (Good Health & Well-being) and SDG 10 (Reduced Inequalities), urging systems that make organ donation equitable, timely, and stigma-free, so no life is lost for want of an organ.
Read More About On Organ Transplantation, Gender Skew
Read More About Organ Transplantation
![]() 14 Aug 2025
14 Aug 2025