World Zoonoses Day 2025 will be marked on July 6 to raise awareness about zoonotic diseases. It will highlight the theme, key infections, and why the One Health approach will be crucial.
World Zoonoses Day: Every year on July 6, the world observes World Zoonoses Day, a crucial global health awareness initiative that underscores the importance of understanding, preventing, and controlling zoonotic diseases. These diseases, also known as zoonoses, are infections transmitted between animals and humans.
With more than 75% of emerging infectious diseases originating from animals—such as COVID-19, rabies, Ebola, and avian flu—World Zoonoses Day serves as a reminder of the urgent need for a One Health approach integrating human, animal, and environmental health efforts.
List Of International National Days 2025 Month-Wise List
World Zoonoses Day 2025 is observed on July 6 to raise awareness about zoonotic diseases—those that spread between animals and humans. This day commemorates the pioneering achievement of Louis Pasteur, who administered the first successful rabies vaccine in 1885.
Source: Wiki
The event serves as a vital reminder of the importance of disease prevention, the interconnectedness of human and animal health, and the global need for collaborative healthcare efforts under the One Health approach.
| World Zoonoses Day 2025 Overview | |
| Particulars | Details |
| Name of the Day | World Zoonoses Day 2025 |
| Date | July 6, 2025 |
| Purpose | To raise awareness about zoonotic diseases and promote their prevention |
| Commemorates | Louis Pasteur’s first successful rabies vaccination in 1885 |
| Significance | Highlights the risk of diseases transmitted between animals and humans |
| Theme (Expected) | To be announced |
| Organizing Bodies | WHO, ISID, FAO, OIE, and national health authorities |
| Key Focus | One Health Approach, Vaccination, Disease Surveillance |
While the World Zoonoses Day 2025 theme has not been officially declared, past themes such as “One World, One Health: Prevent Zoonoses” (2023) and “Preventing the Spread of Zoonotic Diseases” (2024) emphasised collaborative global health efforts. The 2025 theme is expected to follow a similar trajectory, strengthening the need for intersectoral cooperation to curb disease emergence.
The term “zoonoses” (plural of zoonosis) derives from the Greek words Zoon (animal) and Nosos (disease), meaning diseases transmitted between animals and humans. Zoonotic diseases can be caused by bacteria, viruses, parasites, fungi, or even prions.
Zoonotic is an adjective referring to any disease, pathogen, or condition that is capable of being transmitted between species. So, “zoonosis” is the disease, while “zoonotic” describes the type of disease.
| What is the difference between zoonotic and zoonosis disease? “Zoonosis” is the disease (e.g., rabies), while “zoonotic” is the adjective (e.g., zoonotic virus or zoonotic transmission). |
|---|
Zoonotic illnesses can be transmitted in various ways:
Zoonotic diseases, or zoonoses, can be classified based on various criteria such as the type of pathogen, the animal species involved, and the mode of transmission. Understanding these classifications helps in better identification, management, and prevention strategies for zoonotic infections. Here are the main classifications:
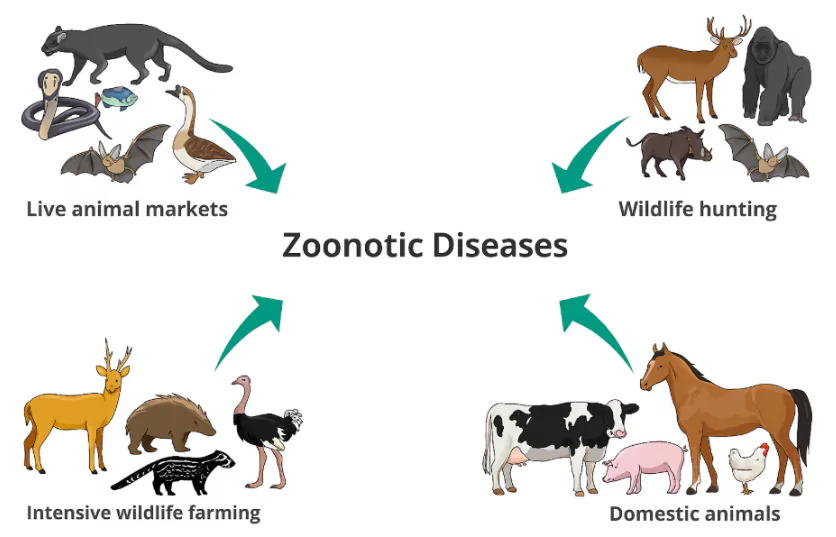
Numerous human behaviours and environmental changes are accelerating the emergence of zoonotic diseases, including:
WHO estimates that 60% of existing infectious diseases and 75% of new emerging infectious diseases are zoonotic in nature.
Though symptoms vary, common signs include:
Early diagnosis is critical to prevent complications or transmission to others.
India has launched several policies and programs to tackle zoonotic threats:
Zoonotic diseases, or zoonoses, are infectious diseases that are transmitted between animals and humans. They can be caused by bacteria, viruses, fungi, or parasites and can spread through direct contact, vectors, food, or environmental contamination. Understanding the wide range of zoonotic diseases is essential for effective prevention, control, and global health preparedness.
Below is a comprehensive list of major zoonotic diseases, their causative organisms, primary reservoirs, and modes of transmission:
| Zoonotic Diseases List | |||
| Disease | Organism | Main Reservoirs | Usual Mode of Transmission to Humans |
| Anthrax | Bacillus anthracis | Livestock, wild animals, environment | Direct contact, ingestion, inhalation |
| Animal influenza | Influenza A viruses | Pigs, other livestock, humans | Direct contact |
| Avian influenza | Influenza A viruses | Poultry, ducks | Direct contact |
| Bovine tuberculosis | Mycobacterium bovis | Cattle | Unpasteurised milk, exposure to infected animals |
| Campylobacteriosis | Campylobacter spp. | Poultry, farm animals | Direct animal contact, raw meat, milk |
| Cat scratch fever | Bartonella henselae | Cats | Bite, scratch |
| Cowpox | Cowpox virus | Rodents | Direct contact (often via cats) |
| Cryptosporidiosis | Cryptosporidium spp. | Cattle, sheep, pets | Contaminated water, direct contact |
| Cysticercosis / Taeniasis | Taenia spp. | Cattle, pigs | Raw/undercooked meat |
| Erysipeloid | Erysipelothrix rhusiopathiae | Pigs, fish, environment | Direct contact, fomites, environment |
| Fish tank / Swimming pool granuloma | Mycobacterium marinum | Fish | Contact with fish or contaminated water |
| Giardiasis | Giardia spp. | Humans, wildlife | Contaminated water, ingestion |
| Haemorrhagic colitis & HUS | Shiga toxin-producing E. coli | Ruminants | Direct contact, foodborne |
| Hantavirus syndromes | Hantaviruses | Rodents | Aerosolised excreta |
| Hepatitis E | Hepatitis E virus | Pigs, wild boar, deer | Undercooked animal meats |
| Hydatid disease | Echinococcus granulosus | Dogs, sheep | Ingestion of eggs excreted by dog |
| Leptospirosis | Leptospira spp. | Rodents, ruminants | Urine-contaminated water or direct contact |
| Listeriosis | Listeria spp. | Cattle, sheep, soil | Dairy products, meat products |
| Louping ill | Louping ill virus | Sheep, grouse | Direct contact, tick bite |
| Lyme disease | Borrelia burgdorferi | Ticks, deer, rodents, sheep | Tick bite |
| Lymphocytic choriomeningitis (LCM) | LCM virus | Rodents | Direct contact |
| Orf | Orf virus | Sheep, goats | Direct contact |
| Ovine chlamydiosis | Chlamydia abortus | Sheep, farm animals | Direct contact, aerosol |
| Pasteurellosis | Pasteurella spp. | Dogs, cats, mammals | Bite/scratch, direct contact |
| Psittacosis | Chlamydia psittaci | Psittacine birds, poultry, ducks | Aerosol, direct contact |
| Q fever | Coxiella burnetii | Cattle, sheep, goats, cats | Aerosol, direct contact, products of conception, fomites |
| Rabies | Rabies virus and other lyssaviruses | Dogs, bats, foxes, cats | Bite or scratch |
| Rat bite fever | Streptobacillus moniliformis | Rats | Bite/scratch, milk, water |
| Ringworm | Dermatophyte fungi | Many animal species | Direct contact |
| Salmonellosis | Salmonella spp. | Poultry, farm animals | Direct animal contact, raw meat, raw foods |
| Streptococcal sepsis (from pigs) | Streptococcus suis | Pigs | Direct contact, meat |
| Streptococcal sepsis (from horses) | Streptococcus zooepidemicus | Horses | Direct contact |
| Toxocariasis | Toxocara canis/catis | Dogs, cats | Ingestion of eggs |
| Toxoplasmosis | Toxoplasma gondii | Cats, ruminants | Ingestion of faecal oocysts, undercooked meat |
| Zoonotic diphtheria | Corynebacterium ulcerans | Cattle, farm animals, dogs | Direct contact, milk |
| Alveolar echinococcosis | Echinococcus multilocularis | Foxes | Ingestion of eggs |
| Brucellosis | Brucella spp. | Cattle, goats, sheep, pigs | Dairy products, milk |
| Crimean-Congo haemorrhagic fever (CCHF) | CCHF virus | Livestock, ticks | Tick bite, direct animal contact |
| Ebola virus disease | Ebola virus | Unknown (possibly bats) | Contact with infected wild animals |
| Glanders | Burkholderia mallei | Horse, donkey, mule | Direct contact, fomites, contaminated food and water |
| Hendra virus infection | Hendra virus | Fruit bats, horses | Exposure to body fluids |
| Kyasanur Forest disease | Kyasanur Forest virus | Rodents, shrews, monkeys | Tick bite, animal contact |
| Lassa fever | Lassa virus | Multimammate rat | Contact with rodent excreta |
| Marburg virus disease | Marburg virus | Bats | Bat exposure |
| MERS (Middle East Respiratory Syndrome) | MERS-CoV | Dromedary camels | Direct or indirect contact |
| Monkeypox | Monkeypox virus | Rodents | Direct contact |
| Nipah virus infection | Nipah virus | Fruit bats | Contaminated food, contact with infected pigs |
| Plague | Yersinia pestis | Rats, fleas | Flea bite, scratch or bite from infected animal |
| Rift Valley fever | Rift Valley fever virus | Cattle, goats, sheep | Mosquito bite, contact with infected animals |
| Tickborne encephalitis | Tickborne encephalitis virus | Rodents, livestock | Tick bite, unpasteurised milk |
| Trichinellosis | Trichinella spiralis | Pigs, wild boar | Raw or undercooked meat |
| Tularemia | Francisella tularensis | Rabbits, wild animals, ticks | Direct contact, aerosol, tick bites |
| West Nile virus infection | West Nile virus | Wild birds, mosquitoes | Mosquito bite |
| Yellow fever | Yellow fever virus | Monkeys | Mosquito bite |
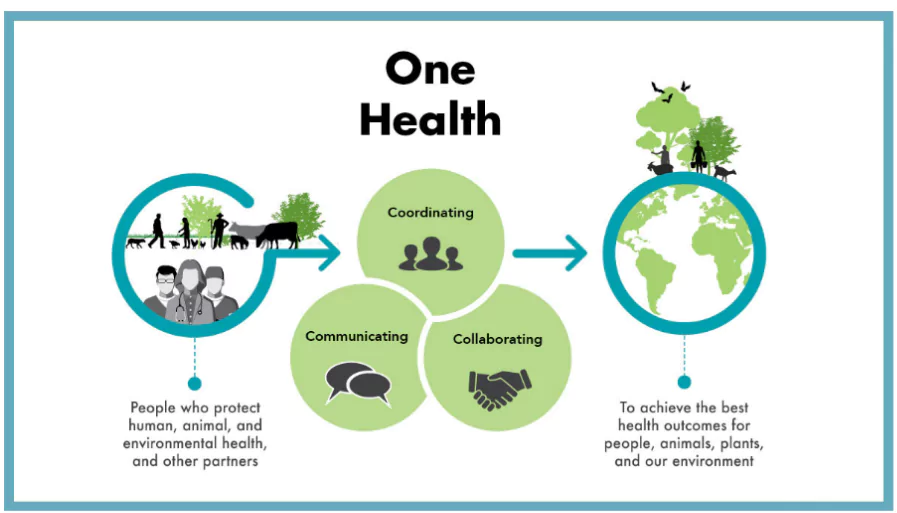
The One Health approach integrates human health, animal health, and environmental health sectors to combat zoonotic disease outbreaks effectively.
World Zoonoses Day 2025 reinforces this concept by encouraging:
Source: cdc.gov
WHO’s OpenWHO platform offers free courses that educate health professionals worldwide on operationalising One Health strategies to combat zoonoses. These include training on:
World Zoonoses Day 2025 is not just a symbolic event. It’s a timely reminder of:
World Zoonoses Day 2025 is not just a date on the calendar—it’s a reminder that our health is intricately linked with the animals and environments around us. With zoonotic diseases posing a growing global threat, especially in the wake of pandemics like COVID-19, promoting scientific collaboration, responsible human behaviour, and the One Health approach is essential for a safer, healthier future.
Ready to boost your UPSC 2025 preparation? Join PW’s UPSC online courses today!
World Zoonoses Day is observed on July 6 to raise awareness about zoonotic diseases and promote health measures to prevent transmission from animals to humans.
The World Zoonoses Day 2025 theme is yet to be officially announced. Past themes have emphasised global cooperation under the One Health framework.
Zoonoses refer to infectious diseases that can spread between animals and humans, caused by viruses, bacteria, parasites, or fungi.
Zoonotic diseases include rabies, brucellosis, Ebola, and avian flu—diseases that originate in animals and can infect humans directly or indirectly.
Zoonosis is the disease itself, while zoonotic is the adjective describing diseases or transmission involving both animals and humans.
Yes. The zoonotic diseases list includes anthrax, rabies, salmonellosis, Lyme disease, leptospirosis, and avian influenza, among others.
<div class="new-fform">
</div>