![]() 25 Jun 2025
25 Jun 2025
UK House Of Commons has passed a bill legalising assisted dying for terminally ill adults, marking a major shift in end of life legislation.
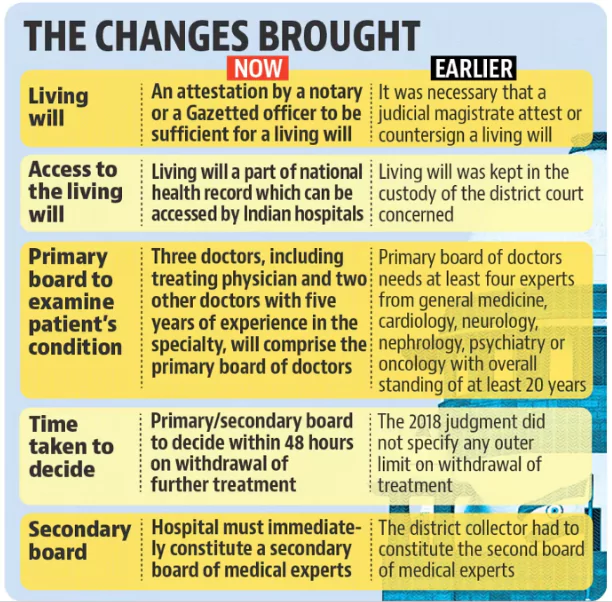 Aruna Shanbaug Case Vs Union Of India (2011): The Supreme Court allowed passive euthanasia in principle for patients in permanent vegetative state but required High Court approval on a case-by-case basis.
Aruna Shanbaug Case Vs Union Of India (2011): The Supreme Court allowed passive euthanasia in principle for patients in permanent vegetative state but required High Court approval on a case-by-case basis.
| Main Practice |
|---|
<div class="new-fform">
</div>
