Context
A study by researchers at Hyderabad, revealed that around 70-80% of people who visit an eye hospital can benefit from teleconsultations, because the severity of their problems did not need attention at a hospital.
| Relevance For Prelims: Telemedicine in India, Digital Health Adoption In India, Global Initiative On Digital Health (GIDH), National Digital Health Mission, Digital Health Adoption In India, Role Of Artificial Intelligence In, and Healthcare, SARAH: A Digital Health Promoter Prototype
Relevance For Mains: Telemedicine in India: Evolution, Key Elements, Benefits, Challenges, and Way Forward. |
Enroll now for UPSC Online Course
About Telemedicine
- Telemedicine is the remote delivery of healthcare services, including consultations and medical diagnostics, over telecommunications infrastructure, allowing patients to access medical care without the need to travel physically.
- This modern healthcare approach leverages digital information and communication technologies, to provide clinical support across distances.
- Telemedicine has emerged as a viable alternative to in-person consultations with doctors in many contexts because it saves patients time and expenses, which can be considerable if they are located in remote areas and/or are not well to do.
Case Study
- Kathirimalai, a tribal village located at a height of 1,200 metres above sea level, in the Chennampatti forest range of Erode had long been denied basic health and education facilities.
- The district administration launched Punnagai (Smile in Tamil), a multi-sectoral tele-facilitation project that uses high-speed 5 GHz wireless systems to provide tele-medicine facilities and linked Kathirimalai with the outside world. The project also focused on online education and skill development for the villagers.
- Thus telemedicine brought specialized healthcare even in the remotest part of the country.
|
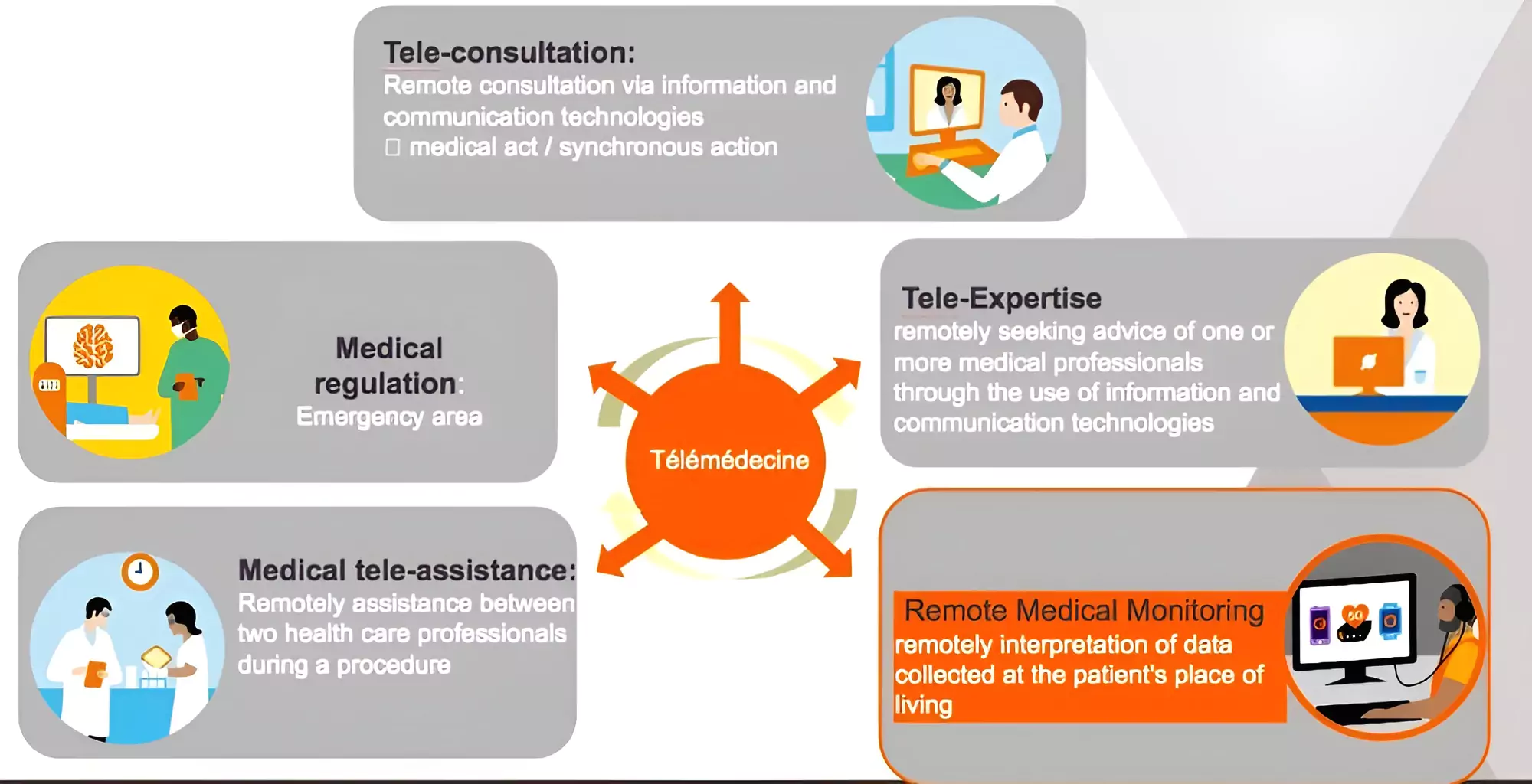
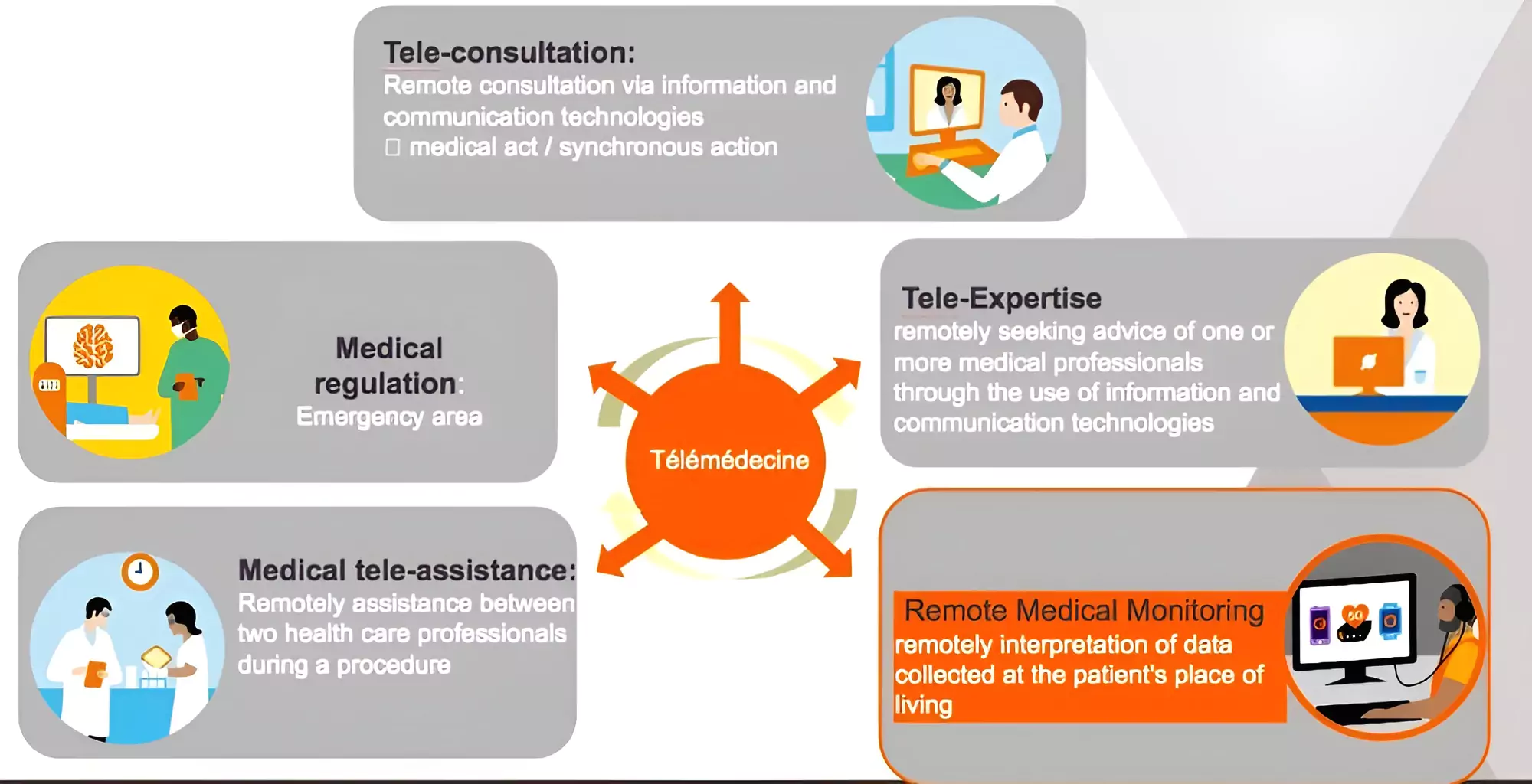
Different Types of Telemedicine Services
- Teleophthalmology: Focuses on eye care and enables patients to consult with ophthalmologists via digital platforms.
- Teledermatology: Remote diagnosis and treatment of skin conditions.
- Telepsychiatry: Deals with mental health issues, providing psychiatric assessments, therapy sessions, and medication management remotely.
- Teleradiology: Involves transmitting radiological patient images, such as X-rays, CT scans, and MRIs, from one location to another for the purposes of sharing studies.
- Telecardiology: Enables cardiac care to be provided through remote monitoring and consultation.
- Telepathology: Involves the practice of pathology at a distance. It uses technology to facilitate the transmission of pathology image-rich data for diagnosis, education, and research.
- Telepediatrics: Allows pediatricians to consult with children and their parents remotely.
- Tele Orthopedics: Provides consultations related to orthopedic conditions.
- Tele-rehabilitation: Aims at improving the physical and psychological rehabilitation process for patients.
- Tele-urgent Care: Tele-urgent care services allow patients to receive immediate consultation for acute but non-life-threatening conditions.
Evolution of Telemedicine
-
Early Developments:
- ISRO’s Telemedicine Pilot (2001): ISRO launched its Telemedicine Pilot Project connecting Chennai’s Apollo Hospital with the Apollo Rural Hospital in Andhra Pradesh.
- Establishment of Telemedicine Networks:By the mid-2000s, several states, including Kerala and Tamil Nadu, started developing their telemedicine networks, often supported by ISRO’s satellite connectivity.
-
Expansion and Integration:
- National Telemedicine Taskforce (2005): The Ministry of Health and Family Welfare established the National Telemedicine Taskforce under the Health Information Technology Board to expand telemedicine across India. It led to the formulation of guidelines and standards for telemedicine practices in India.
- Public-Private Partnerships: Collaborations between government entities and private sector players expanded the reach and technological base of telemedicine services.
Enroll now for UPSC Online Classes
-
Policy Support and Regulation:
- Telemedicine Practice Guidelines (2020): COVID-19 accelerated the need for telemedicine services, prompting the government to release the “Telemedicine Practice Guidelines” in March 2020.
- These guidelines legally enabled registered medical practitioners to provide healthcare using telecommunication and information technologies.
- Digital India Initiative: As part of the broader Digital India initiative, significant emphasis was placed on enhancing digital infrastructure that supports telehealth services.
-
Recent Development:
- Integration with Ayushman Bharat Digital Mission (ABDM): Telemedicine services have been integrated with the ABDM, aiming to create a digital health ecosystem under the National Health Authority.
- COVID-19 Pandemic significantly boosted the use of telemedicine as lockdowns and the risk of infection made traditional visits challenging. It became a critical tool in managing healthcare during the pandemic, with a sharp increase in both service providers and users.
| E-health is an emerging field in the intersection of medical informatics, public health and business, referring to health services and information delivered or enhanced through the Internet and related technologies. |
Key Elements Propelling the Telemedicine Industry’s Expansion
- Healthcare necessity: Chronic diseases are affecting more and more people worldwide. Furthermore, the requirement of healthcare at home has risen due to the geriatric population.
- Technological advancement: Expansion of telehealth solutions is also impacted by prevalence of mobile devices across all age groups and on-demand healthcare apps.
- Easy Diagnosis for patients: Patients are constantly looking for care that is accessible and convenient. Running a telemedicine E Clinic can therefore aid in the timely diagnosis of patients.
- Patient retention: Besides drawing in new patients, it also enables current patients to regularly receive remote checks and guidance.
| China: It has three major telemedicine networks which connect smaller hospitals and clinics in underdeveloped areas with large hospitals.
Mongolia: Nomadic culture of Mongolia results in higher maternal mortality rates. Telemedicine addresses the issue through providing effective maternity services.
Pakistan: Sehat Kahani ( “Story of Health”) initiative empowers female doctors, who are unable to leave their homes to practice and also makes healthcare accessible to rural areas via telemedicine. |
Benefits of Telemedicine
- Bridge Gap Between Urban- Rural Healthcare: Telemedicine can improve access to healthcare services in remote and rural areas, where more than 70% of the Indian population resides.
- Step Towards Universal health coverage: Telemedicine can provide a full continuum of essential health services, from health promotion to prevention, treatment, rehabilitation, and palliative care across the life course enabling universal health coverage.
- Cost Reduction: Telemedicine reduces the need for travel and physical infrastructure, which in turn cuts down healthcare costs significantly.
- A study published by the L.V. Prasad Eye Institute found that teleconsultations saved patients an average of INR 370 to INR 8,339 per visit in travel and related expenses.
- Decrease in Carbon Footprint: The same study from L.V. Prasad Eye Institute noted that teleconsultations resulted in 1,666 fewer kilometers of travel and a reduction of 176.6 kg of CO2 emissions per patient over three months, contributing significantly to environmental sustainability.
- Efficiency and Time Savings: Telemedicine allows for quicker consultations and follow-ups, which saves time for both patients and healthcare providers.
- A survey conducted across several telemedicine platforms in India reported that wait times for teleconsultations were typically less than 10 minutes.
- Enhanced Disease Management: Chronic diseases require ongoing care, and telemedicine facilitates regular monitoring and management without frequent hospital visits.
- For diabetic patients, telemedicine interventions have been shown to help in better glycemic control as patients can regularly consult their doctors for adjustments in their treatment plans.
- Expansion of Specialist Care: Many regions in India lack specialist doctors, particularly in fields such as psychiatry and endocrinology. Telemedicine has enabled access to these specialists without the need for patients to travel long distances.
- For instance, telepsychiatry has expanded rapidly, providing critical mental health services during the COVID-19 pandemic.
- Support for Health Crises: During the COVID-19 pandemic, telemedicine was pivotal in delivering healthcare while minimizing the risk of virus transmission. It supported the healthcare system by providing a means to triage and treat patients remotely, thus alleviating the burden on hospitals.
Enroll now for UPSC Online Course
Challenges Associated with Telemedicine
- Technological Barriers: A significant portion of India’s rural population lacks reliable internet access, which is crucial for effective telemedicine.
- Digital Literacy: Digital literacy remains low in many parts of India, particularly among older populations in rural areas. This affects the ability of patients to use telemedicine services effectively.
- Infrastructure and Equipment Availability: The lack of necessary medical equipment and infrastructure to support telemedicine, such as digital diagnostic tools, is another hurdle. This is especially true in primary healthcare centers in rural areas.
- Regulatory and Legal Issues: There are significant ambiguities in the legal framework governing telemedicine in India, particularly concerning liability, data protection, and cross-border issues.
- The “Telemedicine Practice Guidelines” of 2020 have started to address these, but many areas remain unregulated.
- Privacy and Data Security Concerns: Concerns about the security of patient data and privacy in telemedicine transactions are prominent, especially with the rise in cyber attacks.
- According to a study by a leading cybersecurity firm, healthcare breaches in India saw a 45% jump in 2020 alone.
- Cultural and Behavioral Barriers: A significant portion of the Indian population prefers in-person consultations over virtual ones, driven by cultural norms and the perceived value of physical doctor-patient interactions.
- Integration with Existing Healthcare Systems: Effectively integrating telemedicine with existing healthcare practices and systems poses a challenge, including issues with interoperability and standardization of electronic medical records (EMR).
- Quality of Care: Maintaining the quality of care through telemedicine, ensuring it matches that of in-person consultations, remains a concern, particularly with non-visual examinations and the potential for misdiagnosis.
- Fragmented Insurance Coverage: The coverage of telemedicine by health insurance policies is not comprehensive, which acts as a barrier to its utilization. Patients are less likely to opt for telemedicine options if they are not covered by their insurance plans
Regulatory Framework for Telemedicine in India
- Telemedicine Practice Guidelines, 2020: They provide a comprehensive framework for the practice of telemedicine, including norms for physician-patient interactions, management and treatment protocols, and the privacy and security of patient records..
- National Medical Commission Act, 2019: The act replaces the Indian Medical Council Act, 1956 and influences telemedicine particularly concerning the accreditation, ethical conduct, and professional standards expected from practitioners engaging in telemedicine.
- Information Technology Act, 2000: This act underpins the legal framework for telemedicine as it relates to data protection and privacy. It outlines the obligations for properly handling and protecting electronic health records, which is crucial for maintaining patient confidentiality in telemedicine interactions.
- Drugs and Cosmetics Act, 1940 and Rules, 1945: While primarily regulating the standards for drugs and cosmetics in India, this act also impacts telemedicine especially in the prescription and distribution of medicines over telehealth platforms.
Way Forward
-
Bridging the Digital Divide:
- Infrastructure expansion: Investing in reliable internet connectivity, affordable devices, and digital literacy programs, particularly in rural areas and among vulnerable populations.
- Local language support: Localizing digital health platforms and resources to ensure accessibility and inclusivity.
- Developing user-friendly interfaces: Designing telemedicine platforms that are easy to use and accessible to people with varying levels of digital literacy.
-
Strengthening the Regulatory Framework:
- Developing clear and comprehensive regulations: Establishing data privacy standards, security protocols, and guidelines for data collection, storage, and sharing.
- Promoting interoperability: Implementing standardized data formats and interoperability protocols to enable seamless data exchange between different healthcare systems.
- Creating a robust regulatory body: Establishing a central authority responsible for overseeing the telemedicine ecosystem to ensure compliance with regulations..
-
Fostering Innovation and Collaboration:
- Promoting public-private partnerships: Encouraging collaboration between government, healthcare providers, technology companies, and research institutions to accelerate innovation in the field of telemedicine.
- Supporting startups and entrepreneurs: Providing funding, mentorship, and infrastructure support to startups developing innovative telemedicine technologies.
- Leveraging existing platforms: Integrating telemedicine solutions with existing healthcare infrastructure, such as public health facilities and community health centers.
-
Building Capacity and Expertise:
-
- Investing in training programs: Equipping healthcare professionals with the necessary skills and knowledge to use and manage telemedicine technologies effectively.
- Encouraging knowledge sharing and collaboration: Fostering a culture of knowledge sharing and collaboration among stakeholders in the digital health ecosystem.
Enroll now for UPSC Online Classes
Conclusion
Telemedicine can revolutionize the health industry and paves the way for Universal Health Coverage if the loopholes are effectively plugged.
Also Read: The Debate: Allopathy Vs Ayurveda
| Prelims PYQ (2023):
Consider the following statements:
Statement-I: India’s public sector health care system largely focuses on curative care with limited preventive, promotive and rehabilitative care.
Statement-II: Under India’s decentralized approach to health care delivery, the States are primarily responsible for organizing health services.
Which one of the following is correct in respect of the above statements?
(a) Both Statement-I and Statement-II are correct and StatementII is the correct explanation for Statement-I
(b) Both Statement-I and Statement-II are correct and StatementII is not the correct explanation for Statement-I
(c) Statement-I is correct but StatementII is incorrect
(d) Statement-I is incorrect but Statement-II is correct
Ans: (b) |
![]() 12 Apr 2024
12 Apr 2024